06/10/22
Scale-up insulin access urgently, drugmakers told

By: Syriacus Buguzi
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[DAR ES SALAAM] Drug companies producing insulin must urgently scale up initiatives to tackle the “stark inequity” in access to the life-saving medication for people living with diabetes in low- and middle-income countries (LMICs), a report urges.
Insulin — discovered over 100 years ago — is mainly prescribed to people diagnosed with early-onset type 1 diabetes to help prevent complications and death, but the drug is out of reach for many, says the report released today (6 October) by Access to Medicine Foundation, a Dutch organisation pushing for accountability among pharmaceutical companies.
It comes at a time when cases of diabetes are projected to rise globally to 643 million by 2030, and 783 million by 2045, according to the International Diabetes Federation. The burden of disease is highest in LMICs where 80 per cent of the 463 million adults with diabetes live.
“For children and young adults with type 1 diabetes, where insulin is their lifeline, it must be categorized as essential medicine and be free,”
Kaushik Ramaiya, consultant physician, Shree Hindu Mandal Hospital, Dar es Salaam, Tanzania
The report, which analyses publicly available data, literature and global health policy reports, says only a few drug makers are dominating the insulin market, while gaps persist in access to all forms of insulin.
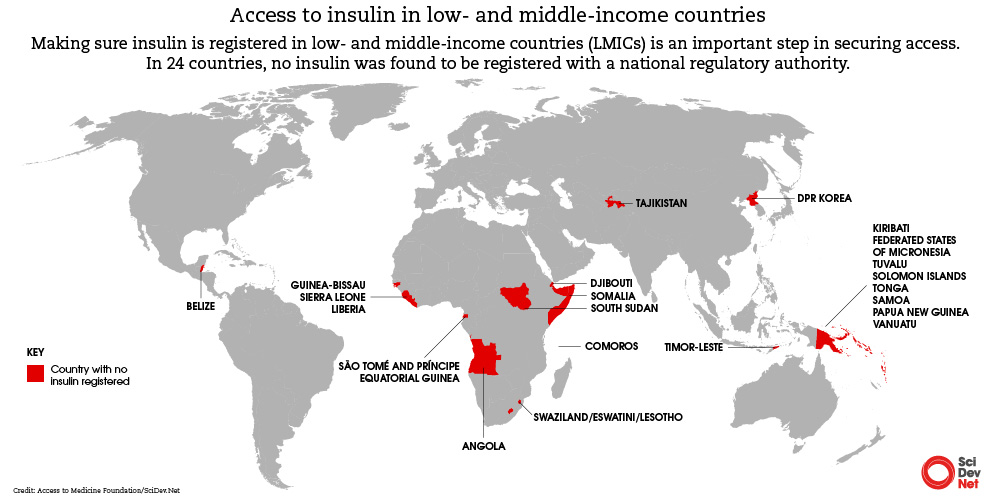
It shows that only 29 countries out of 108 studied have all the insulins classified as “essential medicines” by the World Health Organization, and only one of those is a low-income country. Furthermore, in 24 countries no insulin was registered at all.
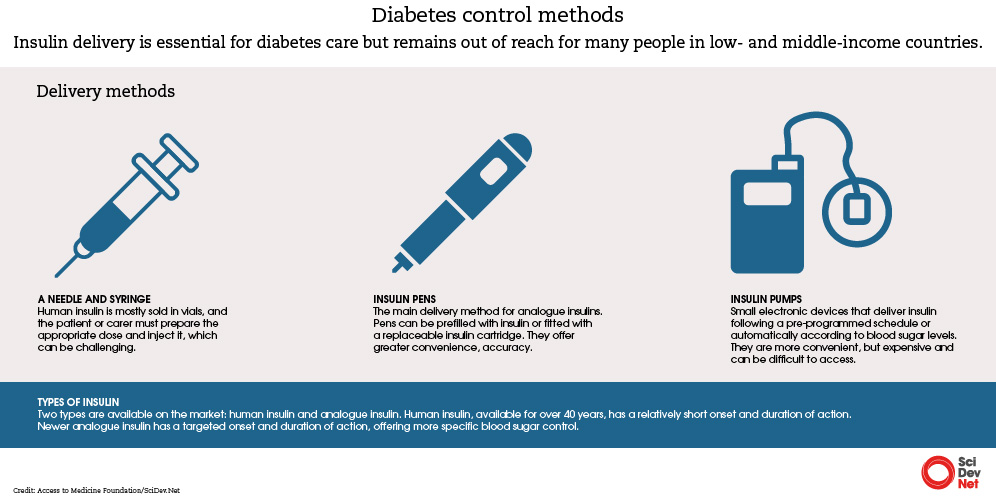
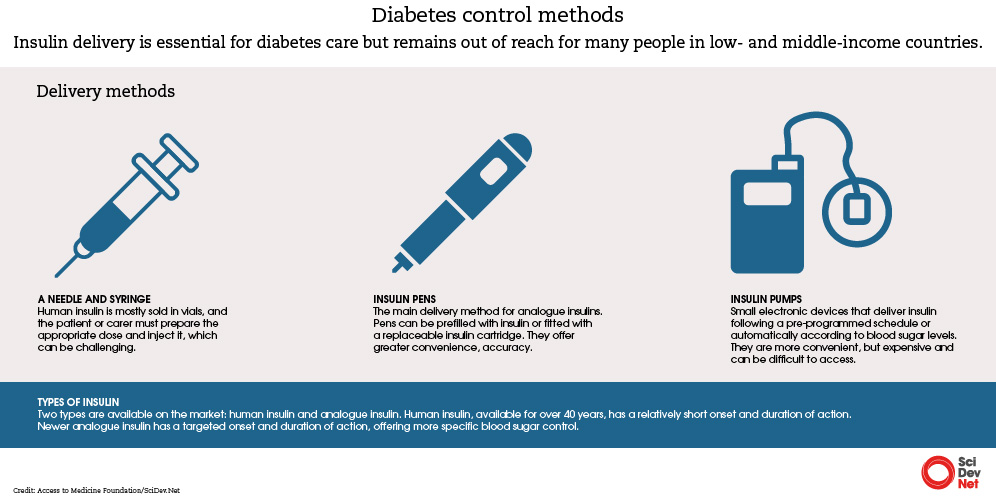
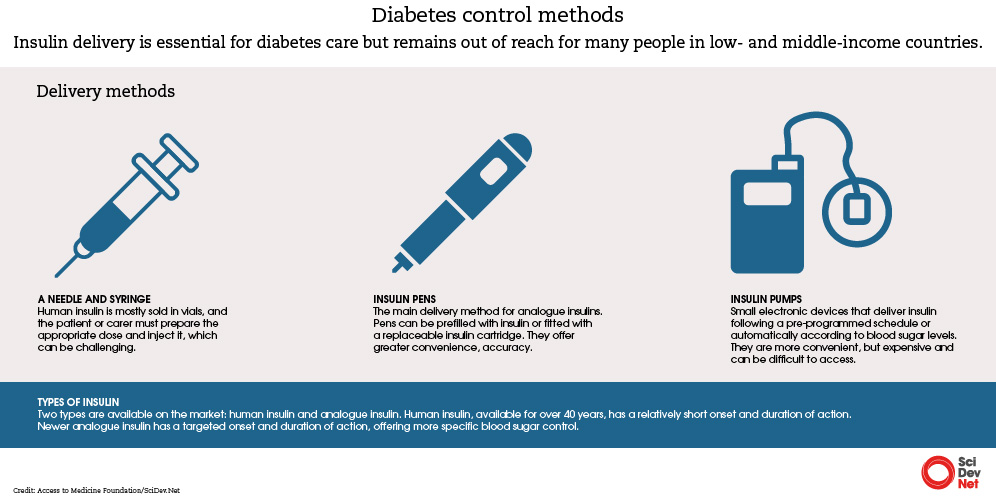
Strategies aimed at making insulin affordable have focused on human insulin, rather than analogue insulin, which controls blood sugar more effectively over a longer period but can cost up to six times more, according to the report.
Ongoing efforts by companies to address gaps in access are “fragmented, and are often focused on a few countries, patient populations and products”, the foundation says. It points to US pharma company Eli Lilly, Denmark’s Novo Nordisk and the French firm Sanofi as the main insulin manufacturers.
Initiatives by these companies to improve access include programmes targeting children, price cap, and equitable pricing policies, but these must go further, the report suggests. Access to other products such as delivery and monitoring tools must also be considered, it says.
“What we want to see as the first step from these companies is to walk away from scattered initiatives and work towards models that ensure more systematic access for patients,” says Claudia Martínez, research programme manager for diabetes and generic medicine at the Access to Medicine Foundation.
Martínez tells SciDev.Net that the report aims to catalyse investment by pharmaceutical companies in solutions such as diversifying products so that people with diabetes can afford the drug and access it “no matter where they live”.
The report points to the need to expand the number and type of insulins on the market in LMICs to boost availability and affordability.
“It’s also important that regulatory bodies include [insulins] in the national medicines lists so that they can make it into the local health systems,” urges Martínez.
For governments, Martínez says: “One thing can be to adopt targets at national level to be able to tackle diabetes […] It’s about taking steps as governments and committing to making diabetes an agenda.”
A spokesman for Novo Nordisk said the company was committed to driving sustainable access and innovation, including through research and development, tackling supply chain issues, and supporting health systems strengthening.
“Increasing access is a complex and ongoing challenge, which is reflected in this report being more demanding than ever,” the spokesman said.
A spokeswoman for Sanofi said the company welcomed “this important report” and would continue its efforts to improve access to diabetes care in LMICs.
“Sanofi has initiatives across commercial, social and philanthropic models to facilitate affordable access to comprehensive diabetes care in LMICs and underserved communities. This includes high-quality analogue insulin products, as well as patient support initiatives and health system strengthening measures, supported by digital tools and health data,” she said.
She said the company also aimed to help address “the multiple barriers to access beyond price”, including research and development, manufacturing, market registration, and procurement, as well as diagnosis and treatment.
Insulin ‘stock-outs’
For people living with diabetes, life can be on the edge in times of insulin shortages. Tanzanian Detricia Pamba, 24, was diagnosed with type 1 diabetes at the age of 13. Missing out on insulin can result in a life-threatening a condition known as Diabetic ketoacidosis.
“I come from a supportive family, and I have health insurance. Paying for insulin is not a problem,” says Pamba, a resident of Dar es Salaam, the country’s commercial capital. “But there are times you go to the hospital and there is a stock-out of insulin and that’s not affecting me alone.
“We end up being divided in groups and given a few weekly doses so that most other people in need don’t miss out completely.
“When it happens that the insulin is not available at the hospital, I need to go to the pharmacy, but there are times the pharmacies also run out of insulin, they call it a seasonal stock-out.
“So, I think the issue here lies in how to increase access of insulin to everyone and at all times,” she tells SciDev.Net.
The Access to Medicine Foundation’s findings show that governments in LMICs are procuring insulin at varying prices, which can lead to high costs.
Natalia Sánchez, a researcher at the foundation, suggests that countries could join pool procurement mechanisms with other countries.
“This could give them more opportunities to negotiate and lower the prices. The other thing they can do is to promote competition within tenders for insulins.”
Kaushik Ramaiya is a consultant physician at Shree Hindu Mandal Hospital in Dar es Salaam and a member of the board of the World Diabetes Foundation. He wants to see free access to insulin in LMICs such as Tanzania, in addition to essential medicine listing.
“For children and young adults with type 1 diabetes, where insulin is their lifeline, it must be categorized as essential medicine and be free,” he says.
Eli Lilly had not responded to SciDev.Net’s request for a response at the time of publication.
This piece was produced by SciDev.Net’s Global desk.