17/11/23
Breakthroughs hailed in childhood TB prevention
By: Claudia Caruana and Ruth Douglas
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Taking a common antibiotic could more than half the risk of children becoming sick with multidrug resistant tuberculosis (MDR-TB), according to findings presented this week at a conference on lung health.
It is one of a number of emerging breakthroughs in the prevention of TB, which kills around 240,000 children each year – the majority of them aged under five.
A single, daily dose of levofloxacin reduced the risk of MDR-TB disease in children by 56 per cent, researchers from the Desmond Tutu TB Centre at South Africa’s Stellenbosch University announced at the Union Conference on Lung Health in Paris on Thursday (16 November).
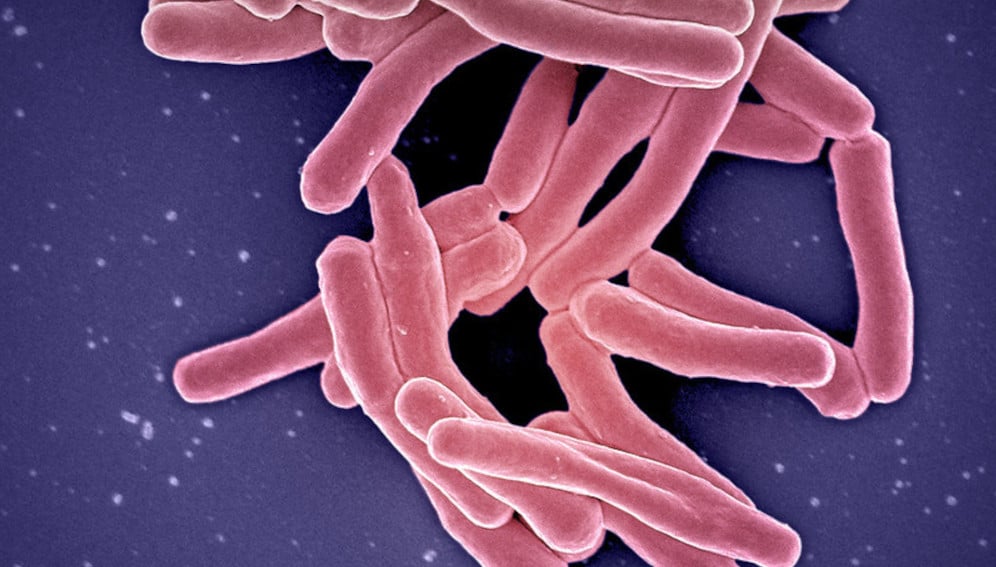
Children are particularly vulnerable to MDR-TB, a form of the disease that has developed resistance to two or more of the first-line drugs used against it.
Because of this resistance, treatment of the disease can be a long and difficult process, which many patients don’t complete. In contrast, this preventative drug comes in the form of a child-friendly, fruit-flavoured tablet, according to the research funder Unitaid.
An estimated two million children a year become newly infected with MDR-TB, which, if left untreated, can develop into what is known as “active TB”, a serious and highly contagious illness that commonly affects the lungs.
“Once it progresses to active disease, multidrug-resistant TB treatment is long and harrowing for children and their families to endure,” said Anneke Hesseling, director of the Desmond Tutu TB Centre and principal investigator of the TB-CHAMP trial, at South Africa’s Stellenbosch University.
“This research provides high-quality evidence to cut that risk in half.” By avoiding lengthy treatments, the intervention could also bring cost savings for national health systems, she added.
The late-stage trial involved 1,000 healthy children who had been exposed to MDR-TB in communities with high burdens of TB and MDR-TB across South Africa.
The conference also heard how a separate human trial had found three new, all-oral, shortened regimens for MDR-TB were safe and effective across all populations, including children, pregnant women and people with other illnesses such as HIV.
The endTB clinical trial, also funded by Unitaid and led by Partners in Health, Médecins Sans Frontières and Interactive Research and Development, found the regimens could reduce treatment time by up to two-thirds compared with conventional treatments, which can last up to two years.
Winnie Byanyima, executive director of UNAIDS, said only about two in five people with drug resistant TB accessed appropriate treatment in 2022, “so it’s great to see these advances in the treatment and prevention of multi-drug resistant TB”.
Only about 2/5 people with drug resistant tuberculosis accessed treatment in 2022. So it’s great to see these advances in the treatment & prevention of multidrug-resistant TB – innovation to save lives & ensure #HealthForAll.#GlobalGoals @UNITAID @StellenboschUni @DesmondTutuTB https://t.co/Yfl5wqreq6
— Winnie Byanyima (@Winnie_Byanyima) November 16, 2023
Finger-prick test
Late last month researchers announced what they said could be a game changer in detecting TB in children, in the form of a simple, rapid analytical tool.
A major reason for the high death toll from TB is the difficulty and delays in diagnosing the disease in children. Most TB tests for adults and children rely on using sputum or phlegm. But small children cannot produce sputum on request. Also, childhood TB has a low bacterial load and non-specific symptoms, often contributing to misdiagnosis or failure to diagnose at an early stage.
The new diagnostic tool requires only a finger prick of blood.
The study, published in The Lancet Infectious Diseases, was led by the Ludwig Maximilian University (LMU) in Munich, Germany, in collaboration with partners from South Africa, Mozambique, Tanzania, Malawi and India.
Laura Olbrich, a medical researcher from LMU and one of the study’s authors, said once diagnosed, 95 per cent of TB cases can be cured.
“So, a test that works on fingerstick blood and can be used without much lab infrastructure, could change the problem substantially,” Olbrich said.
The tool, developed in partnership with US diagnostics company Cepheid and currently at prototype stage, identified almost 60 per cent of children with tuberculosis, with 90-per cent specificity, or accuracy.
“This makes the test comparable with or better than all other tests that work with biomarkers [a biological measure used to detect features of disease],” Olbrich added.
According to paediatric specialist Norbert Heinrich, a co-author of the study, the test has the advantage that the blood sample can be conveniently taken from the fingertip and the results are rapid. “We have the results in just over an hour,” he told SciDev.Net. “For most other tests, the samples must be sent to outside laboratories for analysis.”
“This study is an important step forward toward easier methods to detect TB in children,” said Jacqueline Achkar, a professor of medicine, microbiology, and immunology at the Albert Einstein College of Medicine and an infectious disease physician at Montefiore Medical Center, New York.
“Sputum can be hard to obtain from children…therefore, other tests with body fluids that are easy to obtain are urgently needed,” she told SciDev.Net.
WHO roadmap
On Tuesday (14 November), the World Health Organization (WHO) launched the third edition of its Roadmap towards ending TB in children and adolescents, which sets out a five-year plan to improve prevention, treatment and care of childhood TB.
By 2027, 90 per cent of the estimated number of people with TB should be reached with diagnosis and treatment services, while 90 per cent of people at high-risk of developing TB should be able to access preventive treatment, under the plan.
According to the WHO, TB is the world’s second deadliest disease next to COVID-19, killing 1.3 million in 2022. It is the leading killer among people with HIV.
An estimated 10.6 million people fell ill with TB in 2022, up from 10.3 million in 2021. Most of these were from Asia Pacific and Sub-Saharan Africa.
The WHO says that progress has been insufficient to meet global TB targets set in 2018, stymied by the pandemic and ongoing conflicts.
This piece was produced by SciDev.Net’s Asia Pacific Desk.