20/04/22
mRNA vaccines: facts, figures and the future
By: Fiona Broom
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
mRNA vaccine technology is a field full of promise – as well as unanswered questions – for communities living with the burden of the world’s most deadly infectious diseases.
Despite appearances, mRNA technology is not new. But ever since mRNA vaccines burst onto the global scene to take on COVID-19, a wealth of possibilities has opened up as research teams explore ways to harness mRNA technology to tackle other global health concerns.
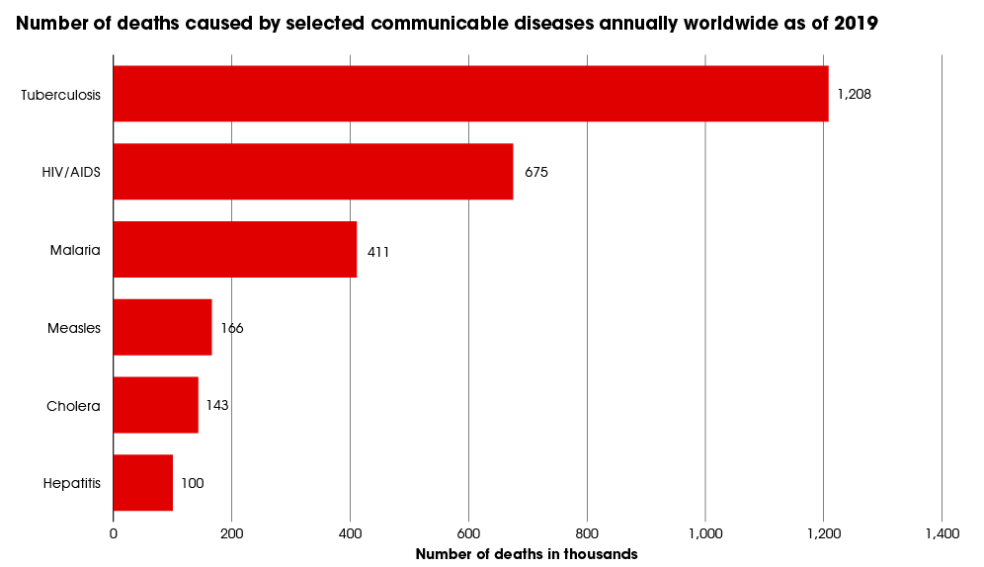
The ‘Big Three’ infectious diseases
Tuberculosis, malaria and HIV are known as the ‘Big Three’ infectious diseases: they are the deadliest communicable diseases in the world. Together, they killed more than 2.8 million people in 2020, according to World Health Organization (WHO) figures. Initial data suggests there were 1.8 million COVID-19 deaths in 2020, although the WHO estimates the number could be “at least” 3 million.
Beyond the deaths caused by the Big Three, almost 290 million people were living with HIV, malaria or TB in 2020. These conditions are known as diseases of poverty. They disproportionately affect developing countries, and they are both a result of and a cause of poverty.
A total of 1.5 million people died from TB in 2020. Globally, it is the second leading infectious killer after COVID-19. An estimated 10 million people fell ill with TB in 2020 – 5.6 million men, 3.3 million women and 1.1 million children. Just eight countries accounted for two-thirds of the total number of TB cases: India has the highest burden, followed by China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa.
Around 627,000 people died of malaria in 2020, with an estimated 241 million cases reported worldwide. Africa carries the majority of the world’s malaria burden – 95 per cent of malaria cases and 96 per cent of malaria deaths. About 80 per cent of malaria infections in this region were in children under five.
Meanwhile, in 2020, 680,000 people died from HIV-related causes. There were 1.5 million new cases of HIV in 2020, while worldwide there were an estimated 37.7 million people living with HIV. The majority of people living with the virus – 25.4 million – are in Africa.
There is no vaccine for HIV, while the first malaria vaccine was recommended for use in children last year. The only licenced TB vaccine is 100 years old and has limited effectiveness.
History of messenger ribonucleic acids
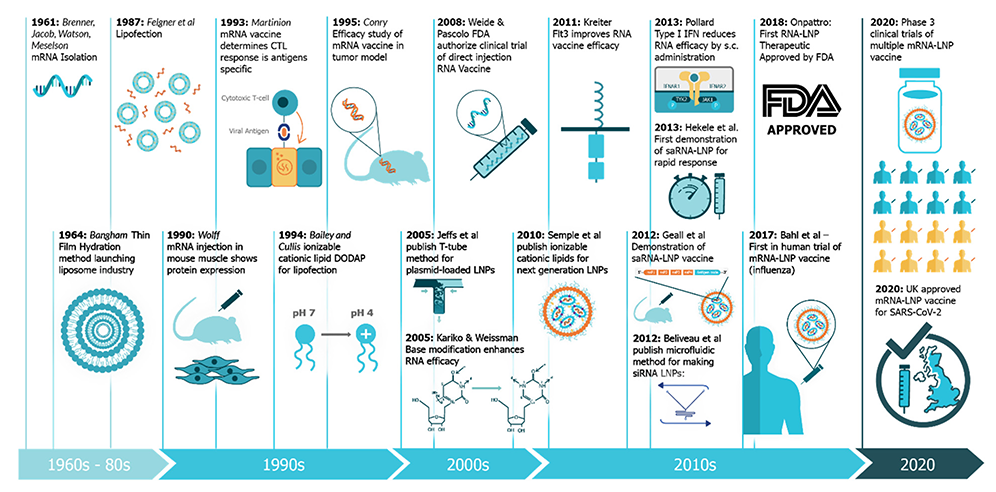
mRNA technology has been in development since the 1960s, but it was proven responsive when SARS-CoV-2 hit the world. Its success in combatting COVID-19 has resulted in renewed interest in developing the technology for other diseases.
In a nutshell, mRNAs are messenger ribonucleic acids that elicit an immune response from cells before degrading. They work by introducing a sequence that is coded for a disease-specific antigen – a substance that causes the body to make antibodies against it; once this antigen is produced within the body, the immune system can recognise it and get ready to fight the real virus, bacteria or parasite.
Before the COVID-19 pandemic, exploration into mRNA vaccines for a range of diseases had begun, including Ebola, Zika and rabies, as well as cancers and influenza.
But the field has developed rapidly in the past few years. In a 2018 review, US-based scientists said that mRNA vaccines represented a promising alternative to conventional vaccine approaches because of their high potency, capacity for rapid development and potential for low-cost manufacture and safe administration.
“The mRNA vaccine field is developing extremely rapidly; a large body of preclinical data has accumulated over the past several years, and multiple human clinical trials have been initiated,” the scientists said. “The data suggest that mRNA vaccines have the potential to solve many of the challenges in vaccine development for both infectious diseases and cancer.”
Why is mRNA technology so exciting?
Interest in mRNA technology has exploded since it entered the mainstream during the COVID-19 pandemic. The full text of one 2020 review of mRNA technology from researchers in Shanghai and Beijing has been viewed around 35,000 times and has more than 40 citations, giving it a high impact factor in the world of scientific literature.
mRNA vaccines appear promising because of the speed with which they can be developed and produced, and their flexibility and adaptability to variants. The US pharmaceutical company Moderna’s mRNA vaccine against SARS-CoV-2 began clinical trials 63 days after the publication of the virus’ genome. By comparison, the Gardasil vaccine for human papillomavirus (HPV) – which uses recombinant DNA technology – took 15 years to be approved for use, in 2006.
Developments in the stability of mRNA vaccines led to the massive increase in interest in the technology. mRNA vaccines were tested in the early 1990s but there were concerns about the scale of production and their fragile stability, according to a 2019 study.
With advances in the synthetic production of mRNAs, the technology became more attractive. Other forms of safe and effective vaccines carry a weakened virus or a part of the virus, and growing the volume of pathogens required to produce immunisations on a large scale, and then weakening the virus, takes time.
With the Coalition for Epidemic Preparedness Innovations (CEPI) setting the world the task of generating vaccines within 100 days of identifying a new germ, research and development groups – including a team at the University of Oxford that has produced a pre-print 100-day vaccine blueprint – say they are up to the challenge.
The future of mRNA vaccine technology
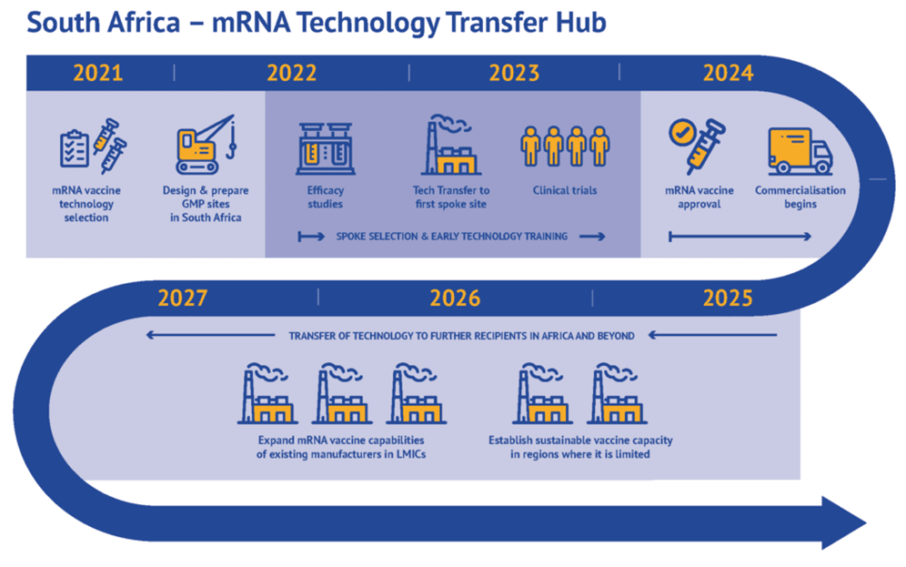
In the first months of 2022 there was a flurry of activity surrounding mRNA technology transfer and development, with the WHO announcing additional locations for its mRNA vaccine technology transfer hubs, and German biotechnology company BioNTech designating sites for new production facilities in Africa.
Amid these announcements, global health leaders and scientists pointed out, time and again, the potential for mRNA to take on the Big Three diseases, as well as non-communicable health burdens such as cancer.
And clinical trials have already begun, or are expected to begin this year, for mRNA vaccine candidates for HIV, malaria, and tuberculosis.
But scientists are tempering their optimism with caution, as reaching the clinical trial stage does not always guarantee a vaccine candidate will be proven safe and effective. And global health advocates say that funding for vaccine research and development, and an ongoing focus on technology transfer and knowledge strengthening in the global South, must continue apace.
The recipes for COVID-19 mRNA vaccines have been tightly held by pharmaceutical companies, who refuse to share patents with developing countries. To combat “vaccine hoarding” and global health inequality, the WHO and a consortium of research organisations and the Medicines Patent Pool banded together in 2021 to unlock the structure of the mRNA vaccines, establishing the first mRNA research centre and transfer hub in South Africa, with ‘spokes’ in Brazil and Argentina.
In February, the WHO announced that six additional countries in Sub-Saharan Africa and North Africa would receive technology to enable them to manufacture COVID-19 vaccines as part of the initiative.
The WHO said that mRNA technology could also be used for insulin to treat diabetes, cancer medicines and, potentially, vaccines for the Big Three deadly infectious diseases. Ultimately, said the WHO, the mRNA tech transfer hubs will promote access to vaccines for everyone, strengthen health security and promote self-reliance for the future.
Kate Stegeman, Africa region advocacy coordinator for the Doctors Without Borders (MSF) Access Campaign, said that diversifying mRNA vaccine manufacturing capacity to low- and middle-income countries should be a global health priority. She said: “More regions producing mRNA vaccines as essential preparedness against infectious diseases could bolster the response not only to COVID-19 and future infectious diseases, but also potentially to existing ones such as malaria, tuberculosis, and HIV.”
This piece was produced by SciDev.Net’s Global desk as part of the Spotlight series ‘The new frontier’.