By: Priya Shetty
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Developing countries must recognise the value of community healthcare and provide clearer ethical guidelines for practice, says Priya Shetty.
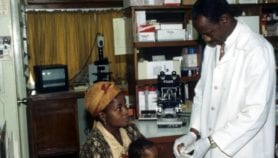
Translating ivory-tower academic research into workable practices on the ground in developing countries is tricky. Health workers on the frontlines of medical care and disease prevention often face huge problems, such as drug shortages, outdated medical equipment, and unreliable transport for traversing remote or hostile terrain.
Programmes that manage to deliver community healthcare are often set up by nongovernmental organisations and tend to be uniquely adapted to local contexts and constraints. But this means they cannot always adhere to the strict codes of practice dictated in UN headquarters.
Community programmes are a pillar of healthcare in poor countries where the conventional health infrastructure is perpetually overwhelmed or inaccessible.
But they tend to be undervalued and under-researched, particularly when it comes to assessing their effectiveness and ethics.
Community programmes
The call for more research to improve health systems in developing nations has been made before and will be given fresh impetus in November at the First Global Symposium on Health Systems Research, co-hosted by the WHO and the Global Forum for Health Research.
Such research is necessary to help establish evidence-based national and international guidelines to advise on what works in practice and what ethical frameworks are appropriate.
Many experts agree that ensuring that health systems research is truly comprehensive provides a major challenge. This means including not only the 'obvious' issues, such as how to improve drug delivery or offer better medical facilities, but also widely ignored ones, such as how to bolster community programmes.
Shenglan Tang of the WHO Special Programme for Research and Training in Tropical Diseases (TDR), who is helping to coordinate the November symposium, told SciDev.Net that even though community health workers are a vital part of the global health taskforce, they remain "half in, half out" of the larger framework.
They are expected to plug essential gaps in healthcare delivery, he says, but command less respect or remuneration than their counterparts in conventional institutions such as hospitals.
One reason is that people on the frontlines of community programmes tend to come from rural villages and are less well educated than other healthcare professionals. Yet being local is the key to their success — as members of the community, they can more easily gain the trust and acceptance of the people they serve.
Ill-educated, not ill health
The constraints that community health programmes operate under necessitate a certain amount of flexibility in the ethical framework.
But there are few guidelines on what ethical compromises can be made. As a result, organisations are left to set their own rules, and this inevitably draws criticism from the global health community.
For example, the most successful way of lowering neonatal mortality in developing nations — home-based neonatal care (HBNC), which was devised in India by social activists Rani and Abhay Bang of the nongovernmental organisation SEARCH — has taken years to be accepted by the WHO and global health community.
This delay was largely because the method relies on poorly educated women to administer neonatal healthcare, and some academics consider this unethical. But the lack of doctors or nurses in many remote villages means that unless women accept poorly educated health workers, their babies will receive no care at all.
A concession to carers' education does not necessarily mean a concession to quality. There is ample evidence that the Bangs' approach works — neonatal mortality rates have dropped by two-thirds in rural villages of Gadchiroli, where the system was pioneered.
Local factors
Bending the ethical rules for community health programmes does not have to compromise the scientific rigour of their evaluation, says Abhay Bang. Methods can still be field tested and scientifically assessed to weigh up their costs and benefits. For example, HBNC underwent field trials in various settings for a decade and the results have been published in journals such as The Lancet.
But poor countries must also incorporate other factors into the equation, says Bang, including disease burden and priority, feasibility, cost, local culture and the availability of healthcare.
When these factors are considered, a drug deemed unethical in the developed world may be appropriate for settings in developing countries. For example, says Bang, the antimicrobial drug co-trimoxazole is not used to treat neonatal infections in the United States, despite field trials that show it to be very effective, because it can, in some cases, aggravate jaundice. But the complication is rare, and because the drug is affordable and does not require cold storage, it is well suited to resource-poor settings.
"Any judgement on the ethics of using co-trimoxazole must consider the other climatic, social and healthcare factors," says Bang.
Without international evidence-based guidance on how to adapt ethical principles to realistic situations, community healthcare providers will continue to face criticism for not meeting international standards of care (however unrealistic these may be).
Running a community health programme poses many challenges, but obtaining the support and scientific guidance of the global health community should not be one of them.
New Scientist, assistant editor at The Lancet, and commissioning editor at SciDev.Net.

Journalist Priya Shetty specialises in developing world issues including health, climate change and human rights. She has worked as a news editor at New Scientist, assistant editor at The Lancet, and commissioning editor at SciDev.Net.