05/01/21
Eyebrows raised over India’s COVID-19 vaccine approval
By: Ranjit Devraj
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
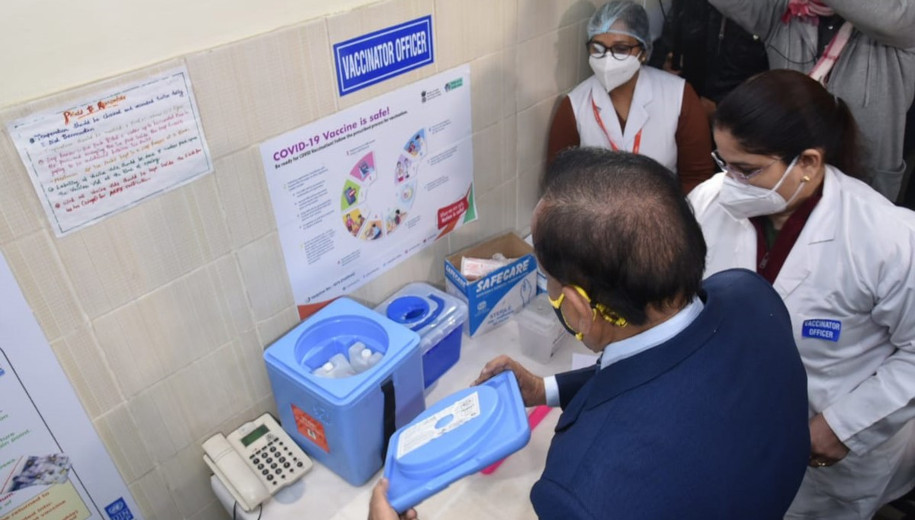
[NEW DELHI] India’s approval for emergency use of a locally developed COVID-19 vaccine that is still undergoing clinical trials has raised a storm of criticism by medical experts and organisations involved in public health.
On Sunday (3 January), the Drugs Controller General of India (DCGI), the main regulatory body, announced approval for Covaxin. The vaccine was developed indigenously by Bharat Biotech in partnership with the state’s Indian Council of Medical Research although it is still undergoing phase 3 human trials and yet to publish data on immunogenicity and efficacy.
DCGI specifically limited Covaxin deployment to ‘clinical trial mode’, a category many experts had problems with. “Never heard of such a category,” Manu Raj, research methodologist and public health researcher attached to the Amrita Institute of Medical Sciences and Research Centre in Kochi, Kerala, tells SciDev.Net.
“It may be a good vaccine but this way of approval casts a shadow on its image”
Manu Raj, Amrita Institute of Medical Sciences and Research Centre
Formal requests for clarifications sent by SciDev.Net to India’s Department of Biotechnology, the government agency supporting the indigenous production of COVID-19 vaccines, were declined.
Also approved for emergency use was the Oxford University-AstraZeneca’s Covishield that uses a weakened adenovirus as a vector to carry the COVID-19 spike protein. The Indian version of Covishield is being manufactured in India by the privately-owned Serum Institute of India.
Following the DCGI announcement, Prime Minister Narendra Modi said in a tweet: “It would make every Indian proud that the two vaccines that have been given emergency use approval are made in India! This shows the eagerness of our scientific community to fulfil the dream of an Aatmanirbhar Bharat (self-reliant India), at the root of which is care and compassion.”
It would make every Indian proud that the two vaccines that have been given emergency use approval are made in India! This shows the eagerness of our scientific community to fulfil the dream of an Aatmanirbhar Bharat, at the root of which is care and compassion.
— Narendra Modi (@narendramodi) January 3, 2021
In a separate tweet, Modi wrote: “A decisive turning point to strengthen a spirited fight! DCGI granting approval to vaccines of Serum Institute of India and Bharat Biotech accelerates the road to a healthier and COVID-free nation. Congratulations India. Congratulations to our hardworking scientists and innovators.”

India Prime Minister Narendra Modi. Image credit: www.kremlin.ru (CC BY 4.0).
Poonam Khetrapal Singh, regional director for WHO South-East Asia, said in a tweet that the organisation welcomed India’s decision to give “emergency use authorization” for COVID-19 vaccines.
“The use of vaccine in prioritised populations, along with the continued implementation of other public health measures and community participation, will be important in reducing impact of COVID-19,” she tweeted.
WHO welcomes India’s decision giving emergency use authorization to #COVID-19 #vaccines –
Dr Poonam Khetrapal Singh, Regional Director,
WHO South-East Asia Region pic.twitter.com/jyQGI6Gymp— WHO South-East Asia (@WHOSEARO) January 3, 2021
But medical scientists and voluntary agencies involved in public health and the rational use of drugs are alarmed at the bypassing of clinical trial protocols and the release of the indigenously developed Covaxin without publishing or publicising trial results.
T. Sundararaman, global coordinator for the People’s Health Movement, an international network of grassroots health organisations, says: “The hasty approval for Covaxin was very unnecessary — they could easily have waited another two months for the completion of phase 3 trials when data and information may have been available. What was the tearing hurry when case incidence in the country was very low?”
A country of 1.3 billion people, India has so far reported 10.3 million COVID-19 cases, second highest in the world, with 150,000 of them fatal. But infection rates have been on the decline after peaking in mid-September.
“It might have been better to take scientists and the public into confidence before releasing it in this manner,” Sundararaman, a former executive director of the National Health Systems Resource Centre of India’s central Ministry of Health and Family Welfare, tells SciDev.Net. He says releasing the vaccine minus data would undermine its credibility and relegate it to a “poor man’s alternative,” even if its efficacy is as good as that of other vaccines.
Raj says: “It may be a good vaccine but this way of approval casts a shadow on its image.” He adds, however, that with the availability of two different vaccines India may be better able to achieve its target of immunising a third of its population over the next six months.
The All India Drug Action Network (AIDAN), an influential drug activists’ group issued a statement asking the DCGI to release all data and analyses on which the decision to launch COVID-19 vaccines was based.
“In the interest of transparency and public welfare, we ask that the regulator [DCGI] share the detailed rationale for the decision along with disclosure of the data, evidence and information that was reviewed by the SEC [subject experts committee] and the data and analysis on the basis of which the REU [restricted emergency use] approval is granted,” the AIDAN statement said.
Mira Shiva, a physician and leader of AIDAN, tells SciDev.Net that the group was “shocked over the decision to grant approval to Bharat Biotech’s Covaxin, while still in clinical trial mode, especially in the context of reports of infection by mutant strains”.
“In contrast, the Oxford University-AstraZeneca vaccine that is being manufactured here by the Serum Institute, was approved in the UK and other countries on the basis of data from rigorous clinical trials,” she says.
According to Shiva, what is at stake is India’s reputation as a major source of reliable and cheap vaccines for the developing world and one controlled by regulatory institutions known for strict conformance to protocols and for carrying out science-based assessments before granting approvals.
Krishna Ella, Bharat Biotech’s managing director, defended his product at virtual press conference on Monday. “Many people are just gossiping. It is just a backlash against Indian companies. That is not right for us. We don’t deserve that. Covaxin has shown less that 10 per cent adverse reactions.”
Covaxin is produced using a whole inactivated virus, the oldest vaccine technique, by which the live virus is killed to so that it can no longer replicate but is still capable of stimulating an immune response in the recipient. Partial phase 1 and 2 trial results for the vaccine are available on company’s website.
Meanwhile, Adar Poonawalla, chief executive officer of Serum Institute of India said in a tweet: “All the risks @SerumInstIndia took with stockpiling the vaccine, have finally paid off. Covishield, India’s first COVID-19 vaccine is approved, safe, effective and ready to roll-out in the coming weeks.”
Poonawalla had earlier announced that his firm, among the world’s largest vaccine manufacturers, had stockpiled close to 50 million doses of Covishield, ahead of clinical trials, and was prepared to make 300 million doses by July 2021.
India has in the pipeline another indigenous COVID-19 vaccine candidate, approved by DCGI for phase 3 clinical trials — a plasmid DNA vaccine called ZyCoV-D developed by Zydus Cadila. DNA vaccines rely on a genetically engineered plasmid (DNA molecule separate from chromosomal DNA and capable of copying itself) that contains the DNA sequence encoding the antigen(s) against which immune response is sought.
“Zydus Cadila completed Phase-I/II clinical trials of this DNA vaccine candidate, in India, in more than 1,000 participants and interim data indicated that the vaccine is safe and immunogenic when three doses were administered intradermally,” a Department of Biotechnology media release said on Sunday.
This piece was produced by SciDev.Net’s Asia & Pacific desk.
* The article was edited on 6 January 2021 to fix typographical errors.