28/04/23
Antimicrobials used on farms ‘weaken human immunity’
By: Sanjeet Bagcchi
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[NEW DELHI] Overuse of antibiotics in agriculture can lead to the emergence of bacteria resistant to the body’s innate immunity, a study led by the University of Oxford suggests.
The research found that an antimicrobial called colistin, which is widely used as an animal growth promoter in farm-raised animals such as pigs and chickens, has likely resulted in the emergence of E.coli strains that can evade the body’s first-line of defence.
Substantial use of colistin in livestock production since 1980, however, led to the development of colistin-resistant E. coli, which harbor mobile colistin resistance (MCR) genes.
Craig MacLean, an author of the study and professor of evolution and microbiology at the UK-based University of Oxford told Scidev.Net: “The use of colistin as a growth promoter has been banned in many countries, but colistin continues to be widely used as an animal growth [promoter] in some countries, particularly in LMICs [low- and middle-income countries].
“This suggests that the risk to human health posed by colistin resistant E. coli will be greatest in LMICs.”
Colistin is a last resort antibiotic — also called an antimicrobial peptide or AMP — used in the treatment of infections by multidrug-resistant bacteria, such as Escherichia coli (E. coli) which causes infections like diarrhea and urinary tract infection.
Substantial use of colistin since 1980, however, led to the development of colistin-resistant E. coli, which harbour genes called mobile colistin resistance (MCR) genes.
This colistin-resistant E. coli is an emerging threat to global public health and is mostly observed in low- and middle-income countries.
It is part of a broader increase in antimicrobial resistance (AMR), which leads to the death of 70,0000 people a year worldwide, according to a report by UN agencies. If no action is taken, the figure is expected to rise to 10 million a year by 2050, while by 2030 AMR could push up to 24 million people into extreme poverty, according to the report.
AMR occurs when microbes or bacteria undergo genetic changes owing to overuse and misuse of antibiotics, making them capable of withstanding the effects of antimicrobials and rendering medical treatments ineffective.
AMPs have a crucial role in combating this. Naturally created in living bodies and holding a key role in innate immunity, AMPs are peptides (protein-like organic substances) with multiple functions. Their biological role inside the body includes elimination of disease-causing microbes, such as bacteria, viruses and fungi.
Some AMPs are used in animals in farms to control infections and as growth promoters, and such use, according to the study, may give rise to cross-resistant bacteria that can overcome the innate immune response in humans.
Innate immune response is the first line of defence in humans to tackle a disease-causing microbe such as bacteria. Development of such cross-resistant bacteria is “highly likely”, the researchers said.
“Our study underscores the importance of not using antimicrobials that are used to treat human infections in agriculture,” said MacLean.
He believes Colistin should be banned as a growth promoter and urges caution in the development of new AMPs.
“Many antimicrobial peptides are under development as potential new medicines to treat human infection,” he added.
“We need to test the impact of resistance to these AMPs on human immunity before they are used therapeutically.”
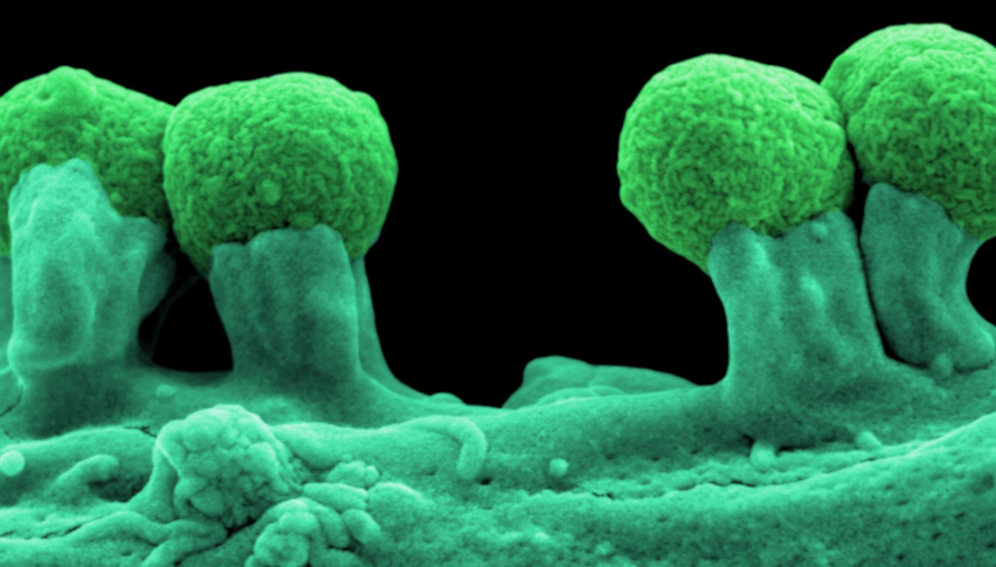
In the study, E. coli bacteria harbouring a type of MCR gene called MCR-1 were exposed to AMPs that contribute to the development of innate immunity in pigs, chickens and humans.
Assessment of the bacteria in terms of their susceptibility to human serum comprising of an antimicrobials cocktail was also carried out.
The researchers found that, owing to the MCR-1 gene in E. coli, the bacteria had an increased resistance to the host (humans) AMPs by 62 per cent, in comparison to the bacteria that did not carry the gene.
Also, the E. coli harboring the MCR-1 gene were at least twice “as resistant to being killed” by human serum.
“This study is the first study to systematically test the impact of MCR-1 on resistance to antimicrobial peptides from humans and agricultural animals,” added MacLean.
George Varghese, a professor at the department of infectious diseases in Christian Medical College, in Vellore, India, who was not involved in the study, said: “What is new about these findings is that they demonstrate how antimicrobial use in livestock production can directly drive the evolution of bacterial resistance.
“This has important implications for how we think about the relationship between antimicrobial use, bacterial evolution, and the emergence of infectious diseases.
Varghese said policymakers and practitioners may need to reconsider how they regulate and monitor antimicrobial use in livestock production in light of the findings.
“This may involve strengthening regulations around the use of antimicrobials in animal feed, implementing surveillance programs to monitor the prevalence of antimicrobial resistance in animal populations, and developing alternative strategies for disease control in livestock that do not rely on antimicrobials,” he added.
This piece was produced by SciDev.Net’s Global desk.















