16/07/19
Poorest children at risk as global vaccination rates stall

By: Inga Vesper
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
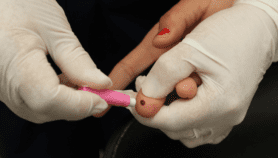
Global vaccination rates for the most common childhood diseases have stalled and remain far from the 95 per cent needed to prevent new outbreaks, UN agencies have warned.
Since 2010, comprehensive vaccination coverage for diphtheria, tetanus and pertussis (DTP3) and measles has hovered at 86 per cent of the world’s children, according to figures released Monday by the World Health Organization (WHO) and the UN children’s agency UNICEF.
In 2018, this meant that 20 million children – one in 10 – around the world failed to get the full dosage of vaccinations needed to protect against these diseases, the agencies said.
“In developing countries, we have seen a wildfire phenomenon, where negative – sometimes politically motivated – social media campaigns scare people away from vaccination,”
Heidi Larson, director, Vaccine Confidence Project
Robin Nandy, chief of immunisation at UNICEF, said the children still missing out on vaccinations are often the hardest to reach.
“These are children in rural locations or in countries with weak health systems,” he told SciDev.Net. “They could be in insecure areas, or in places like urban slums”, where constant migration makes it hard to keep track of children’s health provision.
The data shows that children in the poorest countries suffer from the lowest rates of vaccinations, with Nigeria, India and Pakistan alone accounting for around 7 million unvaccinated children. Countries experiencing prolonged conflict also have low uptake, including Afghanistan, Mali, Somalia, South Sudan, Syria and Yemen.
According to Nandy, the Sub-Saharan African region presents a particular challenge. While vaccination programmes in the region are prospering, growing birth rates mean these programmes struggle to keep up with demand.
The WHO study analysed the incidence of measles—a potentially fatal childhood disease that can cause high fever. Researchers found that, in 2018, the number of reported measles cases more than doubled from the previous year, with 350,000 cases reported.
The disease is on the rise in industrialised nations and in the eastern Pacific, where vaccination rates have not only stagnated but actually declined. Health experts attribute this to a combination of misinformation and complacency.
UNICEF’s executive director, Henrietta Fore, said: “Because measles is so contagious, an outbreak points to communities that are missing out on vaccines due to access, costs or, in some places, complacency. We have to exhaust every effort to immunize every child.”
A recent study by UK-based charitable foundation Wellcome found that one in five people globally lack confidence in the safety of vaccines.
Heidi Larson, director of the UK-based Vaccine Confidence Project, said: “In developing countries, we have seen a wildfire phenomenon, where negative – sometimes politically motivated – social media campaigns scare people away from vaccination. These […] take time and resources to manage, taking a toll on the immunisation programme.”
For the first time, the WHO data covered vaccinations against Human Papilloma Virus (HPV), a sexually transmitted disease that increases the risk of contracting cervical cancer. Researchers found that, in 2018, 90 countries around the world offered the HPV vaccine. However, only 13 of these are low-income countries, and 70 per cent of girls around the world still live out of the vaccine’s reach.
According to the Netherlands-based Access to Medicine Foundation, part of the problem has to do with pricing. While the DTP3 vaccine is available from as little as $0.70 a dose, the HPV vaccine costs around $4.50, even after prices were brought down in 2015 through the global Vaccine Alliance, an initiative to provide low-cost vaccines to developing countries.
Jayasree K. Iyer, executive director of the Access to Medicine Foundation, says HPV is still not well understood worldwide, making parents reluctant to allow their children to be vaccinated. “Diseases such as cervical cancer are also very private,” she said. “In many places reproductive health is not prioritised, and often stigmatised.”The WHO did not issue specific recommendations following the publication of the data, but Nandy believes that improving health systems in general would have a positive impact on vaccination rates.
“Vaccinations are a public health silver bullet, and the large majority of parents want their children to be vaccinated,” he said. “If there is trust in the health system, it will have a positive impact on health-seeking behaviour.”