By: Shahani Singh
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
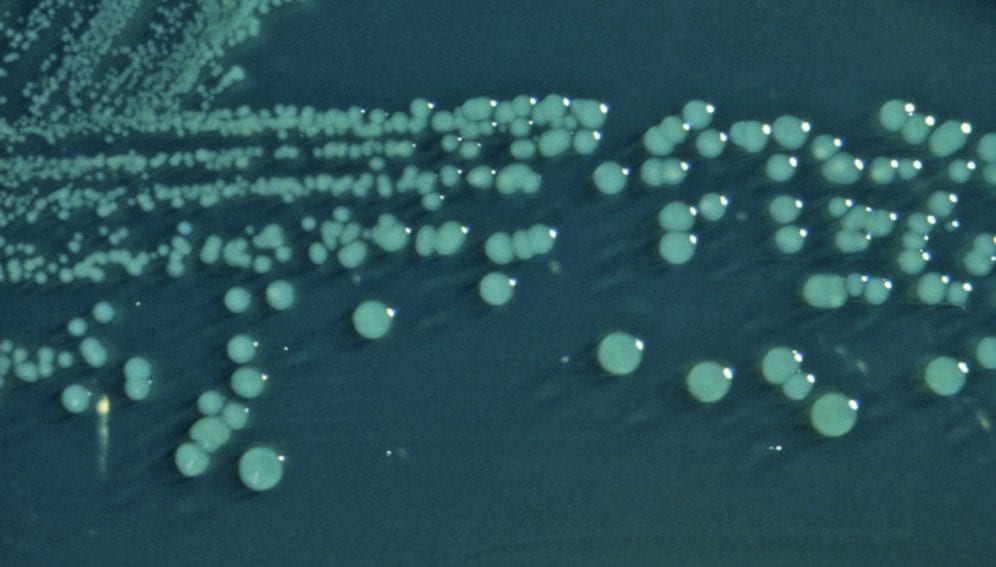
[KATHMANDU] A new study on resistance to antibiotics by the Shigella bacterium, which causes severe dysentery and diarrhoea, indicates the dangers from drug overuse and the importance of continuous surveillance over multi-drug resistant strains.
The study, to be published in the Asian Pacific Journal of Tropical Disease in February, examined resistance patterns in mid- and far-western Nepal to a panel of 15 drugs used in treating shigellosis — an infectious intestinal disease that spreads through water contaminated with faecal matter.
Outbreaks of shigellosis, a major public health problem in developing countries with poor sanitation, have not been officially recorded in Nepal so far, but studies have indicated increased resistance among Shigella species to commonly prescribed antibiotics.
Results of the new study, conducted by the Nepalgunj Medical College (NMC) and Netaji Subhash Chandra Bose Subharti Medical College, India, suggest that drugs such as nalidixic acid, ampicillin, co-trimoxazole and ciprofloxacin should not be used as first-line drugs in the treatment of shigellosis.
“Drugs that have around 90 per cent resistance in a certain population should not be used, whereas those with 50 per cent or less resistance may be used depending on how a patient responds,” says Salman Khan, co-author of the study and assistant professor of microbiology at NMC.
The study is relevant to other South Asian countries where resistance has been observed for the same drugs. “In India, over 70 per cent of Shigella isolates were resistant to two or more drugs including ampicillin and co-trimoxazole during 2002 and 2007," the study says.
Resistance to drugs does not imply removal from distribution. “You cannot eliminate a drug from the distribution channel altogether because in 50 per cent of the cases it might still work,” says Palpasa Kansakar, microbiologist with the National Public Health Laboratory and WHO in Kathmandu.
One cause for increased antibiotic resistance by Shigella was identified as the liberal prescription of drugs and their over-the-counter sales in several developing countries.
“The overuse of certain drugs has not been recorded but, as a physician, I do know that third generation cephalosporins — which should only be used after earlier generation antibiotics fail — are frequently resorted to in Nepal,” Ravi Kiran Kafle, national professional officer at WHO, Kathmandu, tells SciDev.Net.
Nepal is yet to formalise treatment protocols for communicable diseases to allow prescription according to causative agents, disease types and age groups and thereby contain the spread of antibiotic resistance.
Link to the paper in Asian Pacific Journal of Tropical Disease