11/06/20
High resistance to anti-helicobacter drug in Bhutan

By: Saleem Shaikh
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[ISLAMABAD] While over 66 per cent of Bhutan’s population is harbouring Helicobacter pylori bacteria, responsible for ulcers of the gastro-intestinal tract, there is evidence that many of those infected are not getting optimum treatment, a new study suggests.
Bhutan, a Himalayan country of 770,000 people pioneered the Gross National Happiness Index, which guides the country’s economic and social policy and factors in culture and psychological well-being alongside traditional indicators of development such as good living standards, health and education.
“Having analysed the nationally representative data, we discovered that 66.2 per cent of the population is infected with the disease”
Ratha-korn Vilaichone, Thammasat University Hospital
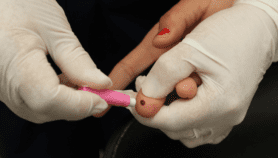
Symptoms of H. pylori infection include pain in the abdomen that worsens when the stomach is empty, nausea, loss of appetite, frequent burping, bloating and weight loss. According to WHO reports, it causes peptic and duodenal ulcers, chronic gastritis and gastric cancer in all age groups.
“Having analysed the nationally representative data, we discovered that 66.2 per cent of the population is infected with the disease,” Ratha-korn Vilaichone, professor of medicine at Thailand’s Thammasat University Hospital, and an author of the study, tells SciDev.Net.
Vilaichone tells SciDev.Net that 81 per cent of the indigenous strains of H. pylori were found resistant to metronidazole, the main antibiotic used to treat gastro-intestinal infections. However, the pathogen was far less resistant to other commonly used antibiotics such as levofloxacin, clarithromycin and tetracycline.
“We observed that frequent antibiotic prescriptions, poor understanding of antibiotic side-effects, bad/inadequate sanitary conditions/practices, use of pit latrines as major toilet facilities, crowded family homes, meagre household spending on health due to low incomes were the key causes of heightened H. pylori prevalence in the country,” Vilaichone says.
The study results, published 29 May in the International Journal of Infectious Diseases, were based on data from examining 1,178 dyspeptic patients — 664 of them female — collected between December 2010 and April 2015 in the six Bhutanese districts of Thimphu, Punakha, Wangdue, Trongsa, Bumthang, and Haa.Punakha district displayed the highest prevalence of the pathogen (85.6 per cent), followed by Wangdue (75.4 per cent) followed by Bumthang (66.1 per cent) and Thimphu (65.7 per cent). Overall, urban areas had higher prevalence than the rural areas.
While prevalence and antibiotic resistance of H. pylori infection varied across regions in Bhutan, the urban area were found to have significantly higher rates of infection than the rural districts.
With evidence for determining the antibiotic resistance pattern now available through the findings of the study, it will be possible to devise a proper treatment regimen for H. pylori infection in Bhutan, the authors suggest.
This piece was produced by SciDev.Net’s Asia & Pacific desk.
•This article was corrected on 16/6/20 to remove quotes erroneously attributed to Rui Paulo de Jesus, WHO representative in Bhutan. SciDev.Net apologises for this error.