By: Halima Athumani
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
After becoming the first university graduate from her “very small” village on Uganda’s Ssese Islands, Diana Nambatya Nsubuga went on to complete a doctorate in public health in the United States.
Now the co-founder of Integrated Health Kwagala Farm, an urban farming foundation that promotes financial independence for women and young people, and a former honorary professor at Makerere University, Nsubuga is an advocate for nutrition, community health and family planning programmes.
Nsubuga tells SciDev.Net why community health workers have the power to change the future of Africa.

Dr. Diana Nambatya. Credit: Kwagala Farms
You hold several global positions and have won numerous awards, and you speak with such passion about both health and farming. But where is your passion stronger?
It was through farming that my parents were able to take me to school, but beyond that, it was through farming that we were able to afford a decent, well-balanced meal, and therefore were able to go through infancy, childhood, with minimal diseases. I’ve learnt in my life that we can’t close this conversation of health when we’re not looking at the multisectoral [approach]. And as a public health specialist, and a professor of public health, I have learned that there are key levers of change.
Number one is nutrition. With nutrition, you can avert over 1,000 deaths in children and mothers. The second one is in immunisation. With immunisation you can prevent so many morbidities and mortalities. The third magic bullet is family planning. And then overarching of all these is community health, community engagement and community ownership.
You are the Africa deputy director in charge of policy and advocacy at the community health non-profit Living Goods. What does your job entail?
My job involves working with African governments, and influencing them to invest in community health. Over 80 per cent of diseases that countries in Sub-Saharan Africa face are preventable. If communities are empowered with the right information and education, they can prevent these diseases. I engage policymakers, parliamentarians, ministers of health and finance, and really convince them to invest in community health, because we’ve seen the biggest lever of change is when communities are engaged, and when communities can own their health.
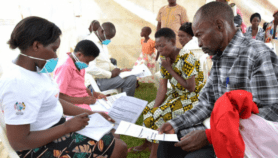
Eighty per cent of community health workers on the continent are women. And so, my role involves … making sure that the community health worker programmes are done in such a way that community health workers are digitally empowered to do their work, they’re equipped, they are supervised, and they are compensated for the work that they do.
Through your engagement with these governments, are they doing what you are advising them to do? Are they supporting the communities?
Community health worker programmes have been in existence for a very long time. But one thing we’ve seen is that different countries are mobilising communities in different ways. For many countries, community health workers are not integrated into the health workforce. Whereas in other countries, community health workers are seen as part of the healthcare team. And so, it depends on what phase the countries are, in terms of the evolvement of their community health worker programme.
For 15 years, you’ve been working as a public health specialist. In regards to maternal and child health in Sub-Saharan Africa, how do you think Uganda and Africa are faring?
I think Uganda has had a journey of its own. We’ve made a lot of progress, particularly in reducing the child mortality, and infant mortality. We’ve also made great strides in reducing the number of women that die during pregnancy and childbirth. That said, there’s still much more that we can do. I look at countries like the UK, where one mother dying during pregnancy and childbirth is a huge thing that causes a [health system] audit.
I look at Uganda … where daily, [the equivalent of] two matatu taxis [which hold about 14 people] full of women die during pregnancy and childbirth. And can I tell you, that does not make news on the continent. It doesn’t make news in my country Uganda.
And a number of factors are at play, because it starts from women understanding that they have the opportunity to plan when to have a child, how often they can have the children, how frequently, and how many.
Who should bear the biggest responsibility for family planning? Is it the government or the community?
Both stakeholders are important. As long as the health of the communities is not in their hands, we still have a long way to go. Government has a mandate to deliver healthcare for its people. But at the same time, government cannot do that alone. Communities — if well sensitised, if services can reach them — will be able to transfer this knowledge, information and services to the people living in the community.
When I look at COVID-19, and the impact it has had on women and girls, COVID-19 has proven to governments that more than ever before, communities need to own their health. And so, it is now time to push and to request countries to continue prioritising community health workers … for transformative health.This interview has been edited for clarity and brevity.