By: Timothy Kitundu
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
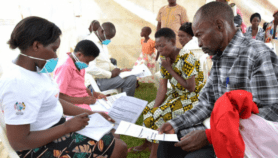
[DAR ES SALAAM] This week Tanzania will launch a fresh strategy to fight malaria by using a new drug that scientists believe can help halve the disease’s incidence and mortality rate by 2010.
The new drug, called ALU, is a combination of the antimalarials artemether and lumefantrine. It will be used together with older drug treatments, some of which have become inefficient at curing the disease.
The health policy will be launched on Friday (15 December).
Every year Tanzania loses an estimated US$10 billion — 3.4 per cent of its gross domestic product — directly or indirectly due to malaria.
ALU is meant to combat malaria parasites that have developed resistance to the drugs chloroquine and sulphurdoxine pyrimethamine, according to Alex Mwita, manager of Tanzania’s National Malaria Control Programme.
"Changing national drug policy remains a sensitive issue that cannot be done overnight," Mwita told SciDev.Net. "However, formulation of the policy systematically involved all stakeholders at all stages."
But Zul Premji, a malaria researcher at the Muhimbili University College of Health Sciences, warns that while ALU is highly effective, it is more expensive than SP and requires a rather high dosage. This could make it difficult for the poor to afford.
The new strategy will stress the proper administration of the drug, a crucial factor in countering drug resistance in the malaria parasite.
To be efficient, ALU must be taken for three consecutive days, and should not be discontinued, even if the patient feels better before that time.
Meanwhile, trials are ongoing for a malaria vaccine that has yielded successful results in the Gambia and Mozambique (see ‘Malaria vaccine shows promising results in children‘).
The vaccine is said to prevent 70 to 80 per cent of cases of malaria in children under the age of one, and lasts for two years. The results of trials carried out in Mozambique and the Gambia were published in The Lancet last year.