08/09/21
Curbing short pregnancy gaps in Africa

By: Royal Uche
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[LAGOS] Chichi Okafor, a 30-year-old Nigerian woman, unexpectedly became pregnant again before her daughter turned six months old.
Although Okafor knew about using condoms to prevent unwanted pregnancies, she felt powerless.
“My husband does not like it, so we resorted to the withdrawal method,” Okafor says. “I am three months pregnant. It has been hell juggling to take care of my daughter and dealing with the new pregnancy.”
The withdrawal method is an old approach for preventing pregnancies by attempting to ensure that ejaculation occurs outside of a woman’s genitals.
“The use of modern contraceptives and optimal breastfeeding can help to reduce the adverse effect of short birth spacing.”
Kehabtimer Shiferaw Kotiso, Wolaita Sodo University
Okafor’s story is an example of how failure to use contraceptives, coupled with short durations of breastfeeding—which can be effective for birth control— is fueling short birth spacing in Sub-Sharan Africa, says Kehabtimer Shiferaw Kotiso, a lecturer at the College of Health Sciences and Medicine at Wolaita Sodo University, in Ethiopia.
The World Health Organization (WHO) recommends waiting at least two years after a live birth and six months after miscarriage or induced termination before having another pregnancy.
But in a study published in PLOS ONE last month involving 496 pregnant women in Northern Ethiopia, 205 fell pregnant in less than 24 months after live birth, with 24 participants getting pregnant less than 12 months after live birth.
According to the study, 196 participants did not use modern contraceptives before their current pregnancy. It found that 108 participants had an unintended pregnancy, with 49 of them breastfeeding their first child for less than 12 months.
Kehabtimer, a co-author of the study, says that in a similar study conducted on 340 women in Port Harcourt, Nigeria, 224 out of 340 pregnant women had short birth spaces.
Kehabtimer explains that short birth space leads to worse child health outcomes, including low birth weight, stillbirth, intellectual disability and developmental delay.
“The use of modern contraceptives and optimal breastfeeding can help to reduce the adverse effect of short birth spacing on maternal and infant health outcomes,” Kehabtimer adds.
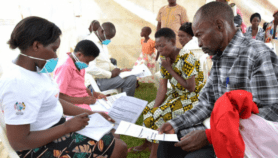
He is calling on the African government to embark on sensitisation campaigns as many African women remain unaware of the benefit of modern contraceptives.
“Stakeholders should find the root causes of why most women who are aware of family planning are not taking up a method and address them,” he tells SciDev.Net.
A 2020 study of eight countries in Sub-Saharan Africa including Nigeria, Tanzania, Uganda and Zimbabwe found significantly shorter birth spacing in Western and Central Africa compared with East and Southern African countries. Chad and the Democratic Republic of Congo had the highest prevalence of short spacing— about 30 per cent and 27 per cent respectively.
“Women who are educated are more likely to favour [a] long birth interval compared to those who are uneducated,” explains the study published in the journal Medicine. “This is not surprising given that educated women are more knowledgeable about contraceptives compared to uneducated women, which will help them to avoid unplanned pregnancy.”
Duduyemi Adeola, state programme coordinator for The Challenge Initiative, in Lagos, tells SciDev.Net that there should be a continuous push for integration of family planning across all maternal, newborn, child and adolescent health, plus nutrition services at the primary health care level, and greater collaboration with the private health sector.
“Behavioural [change] communication activities to address myths and misconceptions about contraceptives, improving the accessibility and coverage of contraceptive use and involvement of men, religious and community leaders in family planning programmes are essential strategies to be considered to avert short birth spaces in Africa,” Adeola says.This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.
References
[1]. Hana Mamo and others Prevalence of short interpregnancy interval and its associated factors among pregnant women in Debre Berhan town, Ethiopia (PLOS ONE 2 August 2021)
[2]. Anthony Idowu Ajayi and Oluwaseyi Dolapo Somefun Patterns and determinants of short and long birth intervals among women in selected sub-Saharan African countries (Medicine, May 2020)