By: Evelyn Otieno
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Treatment success rate among adult patients in Sub-Saharan Africa with tuberculosis that affects the lungs is about 76 per cent, which is less than the WHO target of at least 90 per cent, a study says.
A 2018 report of the WHO says that of ten million people worldwide who had TB in 2017, 1.6 million died, with 25 per cent of the deaths occurring in Africa. In 2017, the treatment success rate globally was 83 per cent.
“Prior to this study, data on treatment success was isolated and inconsistent throughout Sub-Saharan Africa,” says Jonathan Izudi, the lead author of the paper published in BMJ Open this month (6 September). “Therefore we combined available evidence to generate a credible measure of treatment success.”
“We combined available evidence to generate a credible measure of treatment success.”
Jonathan Izudi, Mbarara University of Science and Technology
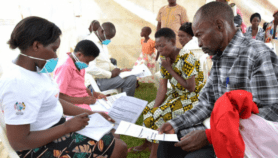
Izudi, a public health researcher at Mbarara University of Science and Technology, Uganda, and other researchers pooled data on treatment outcomes of TB among patients of at least 15 years old in electronic databases including PubMed, Google Scholar and Web of Science. They limited the search to studies conducted in Sub-Saharan Africa and published from 1 July 2008 to 30 June 2018. Researchers also estimated the cure rate of TB across the countries.
The study found that the tuberculosis treatment success rate — defined as proportion of all new tuberculosis cases that a national TB control programme had registered in particular year and had successfully completed treatment
WHO data shows that in Africa, Angola has the lowest TB treatment success rate of 34 per cent and Burundi has the highest success rate of 92. In Asia, China has the highest TB treatment success rate of 94 per cent and Bahrain has the lowest rate of 44 per cent.
Researchers analysed 31 studies with a total sample size of 18,194 participants from seven countries in Sub-Sahara Africa including Ethiopia, Nigeria, Uganda and Zimbabwe.
“We found a pooled cure rate of 64 per cent that varied from 55 to 73 per cent which is substantially lower than WHO recommended cure rate of 85 per cent,” the study says.
Izudi tells SciDev.Net that the he successful treatment of tuberculosis is an important performance target for TB programmes in Sub-Saharan Africa.
Suboptimal treatment success Increase TB transmission at household, community, and public levels, the worst consequence being the emergence of the deadly multi-drug resistant TB,” he explains.
George Onyach a lead clinical officer at the Kenya Red Cross Society, says that Sub-Saharan Africa has recorded high non-completion rates of prescribed TB pills.
“The high number of TB pills per dose and long duration of treatment which ranges between six and 12 months, depending on the type of TB causes non-adherence to prescribed drugs. This contributes to low TB treatment success rate among patients,” Onyach says.
Scientists should reduce the pill burden by giving fewer pills for a shorter duration with the same efficacy and treatment outcome. Additionally, patients should be counselled on adherence, and access to TB treatment [should be] improved.”
“Using this information, policymakers can build capacity, enhance competence, increase the numbers of healthcare workers in TB treatment and increase healthcare budgets for TB care,” he says.
Izudi attributes low TB success rate and cure rates to factors such as advanced patient age, gender, rural residence, the type of TB, HIV status and lack of treatment
The study recommends strategies and TB programmed that will cover the specific needs of patients in Sub-Saharan Africa.
“This calls for a strong multi-stakeholder leadership by healthcare ministries and governments across Sub-Saharan Africa,” Izudi says.
This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.
References
Jonathan Izudi and others Treatment success rate among adult pulmonary tuberculosis patients in Sub-Saharan Africa: a systematic review and meta-analysis (BMJ Open, 6 September 2019)