By: Inga Vesper
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
A global roadmap to eradicate malaria in the next 30 years has been welcomed with caution by scientists and practitioners because of the high extra costs proposed.
The Lancet Commission on malaria eradication used new modelling to predict that, with better malaria interventions and control programmes, the disease could be all but eradicated between 2030 and 2050.
However, to achieve this, global expenditure on tackling malaria must rise by US$2 billion a year, the commission said, in a report published 8 September in The Lancet.
“Whether, and when, eradication is achieved is still an open question, because history tells us that parasite and vector evolution keeps moving the goal posts,”
Sarah Reece, biologist, University of Edinburgh
Combined global spending on malaria eradication reached US$4.3bn in 2016, but fell to US$3.1bn in 2017. Since 2000, the worldwide malaria incidence rate has fallen by 36 per cent, and death rates have plummeted by 60 per cent.
Bruno Moonen, deputy director for malaria at the Bill and Melinda Gates Foundation, which funded the report, said: “There is a recognition that just counting on domestic financing alone is not going to be sufficient.
“The trick will be how to combine prevention methods and treatment in a way that we can get the best return of investment.”
But other experts in the field are doubtful the additional financing can be found, especially in developing countries, where resources are already stretched. James Tibenderana, technical director at the Malaria Consortium, called the funding targets presented in the strategy “unlikely”, pointing out that high expenditures would have to be maintained even as the burden of malaria declines — raising the risk of a resurgence as soon as spending drops.
“Even with increased domestic financing, such as tax-based funding and contributory health insurance, there would still be a substantial gap that will require increased development assistance for health,” he said.
According to the World Health Organization, there were 219 million malaria cases in 2017, and nearly half a million deaths. The strategy proposes a three-pronged approach to eradicate the disease: better implementation of existing malaria control programmes; innovation to develop new tools — such as drugs against resistant parasites and, possibly, a vaccine; and raising spending on the disease by US$2bn a year.
Moonen told SciDev.Net that the creators of the strategy were aware of funding gaps, especially in areas where malaria has declined significantly. “There is a huge benefit in going all the way to zero incidence, because we know that in places where it has been achieved, resurfacing is a lot less likely,” he said. “We need to make sure that resources remain available for countries.”
The Lancet Commission strategy draws on the Global Malaria Eradication Programme, which was launched in 1955 but suspended 50 years ago, in 1969. Moonen says that the programme struggled because it did not take into account drug resistance in malaria parasites, but stresses that it should not be seen as a failure.
“If you look at it from a burden-reduction perspective, there were massive gains,” he said. “Today, we are in a very different place. We know we are seeing multi-drug resistance in some parts of the world, and we have a strong pipeline of new drugs.”
Sarah Reece, a biologist at the University of Edinburgh, who specialises in malaria, told SciDev.Net that there was a need for new tools to treat infections and control disease vectors, but that existing measures could also be employed more efficiently. “Whether, and when, eradication is achieved is still an open question, because history tells us that parasite and vector evolution keeps moving the goal posts,” she said.
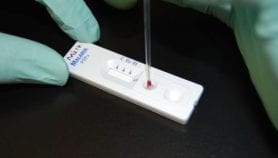
The strategy points out that the largest malaria burden resides in the poorest countries. Just 29 nations, 27 of which are in Africa, accounted for 85 per cent of malaria deaths in 2017. Nigeria and the Democratic Republic of Congo — with large populations and failing healthcare systems — constitute 36 per cent of all global annual cases.Despite repeated calls for extra spending, many doctors in developing countries still rely on traditional methods to combat malaria. Julius Mollel, a general surgeon at Nkoaranga Hospital in Tanzania, said that in Zanzibar, where no new cases of malaria were reported this year, success has been achieved through supplying health centres with test kits and giving away free insecticide-treated mosquito nets to pregnant women and children under five.
“I don’t think it is possible to eradicate malaria globally,” said Mollel. “In Tanzania, it is still among the top ten diseases, especially in children.”
This story was originally published by SciDev.Net's global edition.