12/11/19
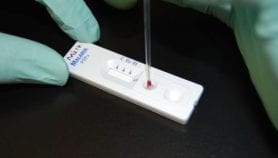
Africa study links malaria gene to blood disease

Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[NAIROBI] The biggest genome study of Africans ever conducted has shown a link between genes that confer resistance to severe malaria and blood diseases such as sickle cell anaemia, raising the possibility of new treatments.
“Examples include genetic variants that cause diseases such as thalassemia and sickle cell anaemia that are more common in African populations living in regions endemic for malaria,” study co-author Segun Fatumo, an assistant professor at the UK-based London School of Hygiene & Tropical Medicine, tells SciDev.Net.
In these regions, genetic variants that would ordinarily cause harm due to disease are selected because they also protect against diseases such as severe malaria, he explains.
“Studying diverse populations exposed to different histories and environments can provide unique opportunities to study genetic associations with disease.”
Segun Fatumo, London School of Hygiene & Tropical Medicine
Whereas the genetic make-up of individuals from Western populations have been well studied, genetic studies focusing on Africans have been very limited.
The study identified an association between a genetic variant which reduces the production of a form of red pigment of blood called alpha-thalassemia among Africans, and glycated haemoglobin — a form of red pigment of blood that is chemically linked to sugar levels.
Because glycated haemoglobin is commonly used to diagnose diabetes, Fatumo explains, this also raises concerns that glycated haemoglobin may not be a good test for diabetes in these populations.
The study combined genome sequencing of 6,400 individuals from Uganda and analysis of genomic data from 14,000 additional individuals from Ghana, Kenya, Nigeria, South Africa and Uganda, the researchers identified new genes associated with cardiovascular or heart-related diseases, according to the study published in the journal Cell last month (31 October).
Finding new associations may lead to identification of novel drug targets, adds Fatumo, who is also a senior scientist at the Medical Research Centre Unit in Uganda.
The study that took 11 years from 2008 built on the long-standing research programme of Uganda’s Medical Research Centre to establish a genomic data resource to understand the broad determinants of population health and disease in the region.
This study, Segun tells SciDev.Net, is important in the global context as analysing African ancestries would ensure equity of benefit of genetic studies.
Richard O. Oduor, a molecular biologist with a background in drug discovery and a senior lecturer in the Department of Biochemistry, Microbiology and Biotechnology at Kenya’s Kenyatta University, says the study brings new insights to the manner African continent should approach its rising disease burden.
”A drug functions through a mechanism of action that targets one or several intervention points commonly referred to as drug targets,” explains Oduor. “Often, these drug targets are influenced by genomic activities of the cell, and are largely expected to be similar across populations.”
He adds that with these new findings on genetic variations it can no longer be assumed that the drugs targets and disease indicators validated for diagnosis in one population would be applicable in another.This finding should gain rapid traction within African governments because most drugs currently commercialised in Africa were developed in the West, and with limited knowledge of genetic variations in African populations.
Such drugs may become less efficacious or non-responsive to the intended disease condition despite the huge resources involved in their purchase.
“African countries can no longer expect the West [to] develop drugs that are unique to the African population,” Odour explains. “African governments must now put resources in drug discovery.”
This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.
References
Deepti Gurdasani and others Uganda genome resource enables insights into population history and genomic discovery in Africa (Journals Cell, 31 October 2019)