By: Sam Otieno
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[NAIROBI] Investing in low-cost technological innovations and tools could reduce malaria burden in Africa, say experts.
Speaking at a workshop on closing gaps to protect people from deadly forms of malaria held in Kenya this month (21 April) — barely a week before World Malaria Day today (25 April), the experts emphasised that Africa bears the greatest malaria burden worldwide.
According to the WHO, about 429,000 people died from the disease in 2015 globally, majority of them being young children in Sub-Saharan Africa.
Nathan Bakyaita, malaria advisor at WHO in Kenya, tells SciDev.Net that despite recent investments in malaria prevention and control in Kenya, malaria remains a major public health threat, causing an estimated 6.5 million infections and 12,000 deaths annually.
“African governments should embrace preventive measures, educate and raise awareness to communities, in order to be equipped with information on how to reduce the gap.”
Rose Jalang’o, Kenya’s Ministry of Health
“Malaria prevention tools, including insecticide-treated mosquito nets (ITNs), indoor residual spraying (IRS) and preventive therapies are powerful and cost-effective,” notes Bakyaita.
He says some of these tools are saving lives, but are still unavailable to many who need them. For instance, 43 per cent of people at risk of malaria are not protected by either ITNs or IRS while 69 per cent of pregnant women are not accessing the WHO-recommended three or more doses of preventive therapy in Africa.
But Bakyaita is urging countries and their development partners to urgently improve access to these life-saving prevention tools as that will help in closing the gap.
According to WHO Africa Regional Director, Matshidiso Moeti, malaria vaccine could be available once phase III of malaria vaccine RTS,S is completed in 2018.
“I am excited to tell you that right now, malaria vaccines are looking very promising, with more than 20 candidate vaccines in various stages of development,” she says.
Eliane Furrer, WHO technical officer, initiative for vaccine research, says that Ghana, Kenya and Malawi will take part in a WHO-coordinated RTS,S malaria vaccine implementation programme that is expected to make the world’s first malaria vaccine available in selected areas, beginning 2018.
“This will provide experience to Kenya for potential future roll-out and together with information from the other countries, [and] enable a WHO recommendation on potential wider scale use of the vaccine in Sub-Saharan Africa,” Furrer explains.
She adds that the countries were selected based on well-functioning malaria and immunisation programmes, with good coverage of recommended malaria control interventions and childhood vaccinations and desire to engage in the vaccine programme by national stakeholders.
But Furrer notes that the vaccine should complement and not replace existing malaria prevention, diagnostic and treatment tools.
Rose Jalang’o, a programme officer with national vaccines and immunisation programme in Kenya’s Ministry of Health, concurs with Furrer, saying suitable interventions should be implemented in in areas where malaria threat is common so as to reduce the parasite.
“African governments should embrace preventive measures, educate and raise awareness to communities, in order to be equipped with information on how to reduce the gap,” says Jalang’o.
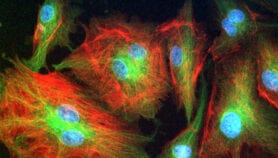
Patricia Njuguna, chair of clinical research, Kenya-based KEMRI-Wellcome Trust, explains that RTS,S is an added advantage as it aims to trigger the immune system to defend against the first stages when malaria parasite enters the human host’s bloodstream through a mosquito bite and infects the liver.“Also the vaccine is designed to prevent the parasite from infecting the liver, where it can mature, multiply, re-enter the bloodstream, and infect red blood cells, which can lead to disease symptoms,” Njuguna adds.
This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.