24/07/20
HIV, malaria, TB deaths could rise by up to 36 per cent

Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
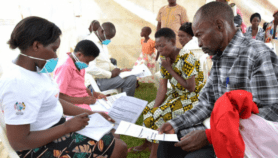
[NAIROBI] Low- and middle-income countries could see HIV, tuberculosis (TB), and malaria deaths increase by up to 36 per cent over the next five years because of COVID-19-induced health services disruptions, a study projects.
According to the 2019 World Malaria Report, an estimated 228 million cases of malaria occurred worldwide in 2018, with the World Health Organization (WHO) African Region reporting 213 million cases, or 93 per cent.
In 2017, about 2.5 million people contracted TB in Sub-Saharan Africa and 665,000 of them died from the disease.
The study forecasts that without access to antiretroviral therapy for HIV, timely TB diagnosis and treatment, and provision of long-lasting insecticide-treated nets for malaria during the COVID-19 pandemic, HIV deaths could go up by 10 per cent, with figures for TB and malaria being 20 and 36 per cent respectively.
“Millions of people rely on services for HIV, TB and malaria and we are concerned about the impact that such disruptions would cause,” says Timothy Hallett, a co-author of the study and professor of global health at the UK-based Imperial College London.
“Millions of people rely on services for HIV, TB and malaria and we are concerned about the impact that such disruptions would cause.”
Timothy Hallet, Imperial College London
He explains that epidemics can cause knock-on consequences for health services if people are unable or unwilling to seek care, or if health systems become overwhelmed.
“During the Ebola epidemic in Guinea in 2014, more additional people died from malaria that year due to fewer malaria treatments being administered than died from Ebola,” the study says.
Hallett says that in many Sub-Saharan African countries, HIV, TB and malaria are among the most common causes of death.
“Significant declines have been recorded in recent years in many places though, thanks to programmes that have been scaled-up,” he says.
Researchers used a computer model to create different scenarios to examine the effects of different policies on HIV, TB and malaria deaths.
“Our results underscore the extraordinarily difficult decisions facing policymakers. Well managed, long-term suppression interventions could avert the most deaths through avoiding a COVID-19 pandemic,” says the study published in the Lancet Global Health this month (13 July). “However, if the interventions are not well managed, they could lead to a large spike in deaths from other causes.”
Hallett tells SciDev.Net that interventions to minimise the impact include maintaining treatment for those on antiretroviral therapy, continuing timely diagnosis and initiation of treatment for TB and continuation of bed net distribution.
“But these should be done in a way that does not increase the risk of COVID-19 transmission,” he says. “Specifically, for HIV, to avoid the need for multiple visits to pharmacies, the major recommendation is to move to multi-month prescriptions, if stock levels allow.”
Dawood adds that taking delivery systems to patients, such as through mobile clinics and courier services, are among the most important considerations.
“The findings are important in that it informs planning for possible impact under different scenarios. It also highlights the need for urgent intervention in these challenging times,” says Dawood, who was not involved in the study.
This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.
References
Alexandra B. Hogan and others Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study (The Lancet Global Health, 13 July, 2020)