Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Safe, reliable medicines could help Africa fight antimicrobial resistance, argues Elizabeth Shekalaghe.
We’re in a public health crisis: resistance to our drugs is rapidly mounting while patients are suffering because they can’t access adequate healthcare.
Today, antimicrobial resistance and universal health coverage — the concept that people should be able to access healthcare without suffering financial hardships— are fixtures at the top of the African and global health agenda. And for good reason.
In some countries, an estimated 40 per cent of infections are already resistant to antibiotics, and 11 million Africans are pushed into poverty every year due to skyrocketing health expenses.
“We know that poor-quality medicines can drive drug resistance.”
Elizabeth Shekalaghe, Tanzania’s Pharmacy Council
Last month (23 September), the UN convened a high-level meeting on universal health coverage during its annual general assembly in New York, United States. At the meeting, countries issued financial and political commitments to accelerate progress on our collective goal of ‘health for all’, which includes combatting antimicrobial resistance, a phenomenon which occurs when medicines can no longer fight infections caused by microbes such as bacteria.
Reliable medicines vital
As we work to address our twin priorities of antimicrobial resistance and universal health coverage, one factor is key to accelerating progress: better access to safe and quality medicines.
Across low- and middle-income countries, an estimated one in ten medicines is substandard or falsified. Here in Africa, that number is nearly double – and our patients are paying the price.
Consider a mother whose child develops flu-like symptoms. Desperate for help, she brings her child to the nearest pharmacy where she’s told he likely has pneumonia and is given antibiotics. After a few days, the child’s health worsens so she takes another day off work and this time travels to the clinic, where lab results show that the child’s pneumonia is resistant to the antibiotics.
We know that poor-quality medicines can drive drug resistance when they deliver insufficient active ingredients, allowing microbes such as bacteria and viruses to adapt and outsmart common treatments.
There are myriad reasons medicines may degrade – and while medicines standards have improved in some countries such as Tanzania, power outages, improper storage and exposure to sunlight, are just some of the factors that have the potential to render medicines ineffective.
This impacts not only health and lives but economies too.
On average, medicines account for a quarter of national health spending, with estimates as high as two-thirds in some low- and middle-income countries.
Sadly, every year, US$30.5 billion of this is wasted delivering medicines that don't work, making medicines among the leading sources of wasted health spending worldwide.
Fighting poor-quality drugs
The good news is that we know how to mitigate the spread of poor-quality medicines, and there’s increasing acknowledgement of the linkages between quality and both antimicrobial resistance and universal health coverage.
“Governments must commit to building more resilient regulatory systems.”
Elizabeth Shekalaghe, Tanzania’s Pharmacy Council
Earlier this year, an independent, UN-commissioned report on the global antimicrobial resistance crisis called for equitable and affordable access to quality antimicrobials, as well better surveillance to monitor the spread of resistance.
Also a political declaration that countries issued at the high-level meeting on universal health coverage calls for universal access to safe, affordable, effective and quality medicines, and outlines five key actions to realise this goal. And a global campaign known as Medicines We Can Trust has hundreds of partners around the world working to address the challenge of poor-quality medicines.
We’ve also seen countries begin to take concrete actions to integrate quality assurance within their antimicrobial resistance and universal health coverage agenda. In July, I attended the ReAct Africa Annual Conference in Kenya where participants from 33 African countries discussed efforts to develop national antimicrobial resistance action plans and initiatives to advance universal health coverage and ways to tackle the problem of poor-quality medicines.
I shared the experience of my home country of Tanzania, where we’ve worked to strengthen our drug regulatory system, which is key to protecting quality at every step of a medicine’s life span, from the manufacturing plant to the hospital shelf. Last year, the Tanzania Drug and Medicinal Authority (previously the Tanzania Food and Drug Authority) became the first in the region to be certified by the WHO as a well-functioning, regulatory system for medical products.
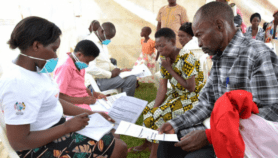
The programme seeks to improve access to affordable, quality medicines and pharmaceutical services in areas where there are few or no registered pharmacies, which includes rural areas.
Other African countries such as Liberia and Uganda have also followed our model of accrediting medicine dispensing outlets to make quality medicines and services available to people living in underserved areas.
How to sustain progress
For sustained progress, we need to scale up these kinds of efforts across the region.
Governments must commit to building more resilient regulatory systems. Critical to this is ensuring that individuals throughout our supply chains have the skills they need to be good stewards of quality – the logisticians tracking medicines supply, the chemists who evaluate medical products and the doctors who interface with our patients. Organisations such as the WHO and the United States Pharmacopeia are helping us get there by facilitating the creation of stronger quality assurance systems and providing hands-on training to prevent, detect and respond to poor-quality medicines.
As we all work to realise the goal of ‘health for all,’ we face difficult decisions about where to prioritise efforts and funding but we cannot afford to cut corners on quality.
As the WHO regional director for Africa Matshidiso Moeti has cautioned, “access to medicines alone, without quality assurance, is not enough”.
We can and must take concrete action now – action that will have a far-reaching impact and allow us to achieve our shared ambitious goals for a healthier world.
Elizabeth Shekalaghe is the registrar of Tanzania’s Pharmacy Council, Ministry of Health, Community Development, Gender, Elderly and Children. She can be reached at [email protected]
This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.
References
[1] Stemming the superbug tide: Just a few dollars more (OECD, 2018).
[2] UHC in Africa: A framework for action (The World Bank, JICA, Global Fund and WHO, nd)
[3] WHO global surveillance and monitoring system for substandard and falsified medical products (WHO, 2017)
[4] Sachiko Ozawa and others Prevalence and estimated economic burden of substandard and falsified medicines in low- and middle-income countries (JAMA Network Open, 10 August 2018)
[5] Maryam Bigdeli and others Medicines and universal health coverage: challenges and opportunities (Journal of Pharmaceutical Policy and Practice, 16 February 2015)
[6] WHO global surveillance and monitoring system for substandard and falsified medical products (WHO, 2017)
[7] Anita K Wagner and others Quality use of medicines within universal health coverage: challenges and opportunities (BMC Health Services Research, 27 August 2014)
[8] No time to wait: Securing the future from drug-resistant infections (Interagency Coordination Group on Antimicrobial Resistance, April 2019)
[9] Political declaration of the high-level meeting on universal health coverage “universal health coverage: moving together to build a healthier world” (UN, 23 September 2019)
[10] Everyone should have access to medicines they can trust (Medicines We Can Trust, nd)
[11] Edmund Rutta Medicines in health systems: Advancing access, affordability and appropriate use (Management Sciences for Health, 2014)
[12]Tanzania is first African country to reach an important milestone in the regulation of medicines (WHO Africa Region, 10 December 2018)