By: Jacquie Ogada
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[NAIROBI] About 28 million people could fall into extreme poverty by 2050 if high antimicrobial resistance is not addressed, a meeting has heard.
Antimicrobial resistance occurs when medicines for controlling infections caused by germs such as bacteria, fungi, viruses and parasites are no longer effective. According to the World Bank, antimicrobial resistance could cut annual global gross domestic product by about US$1 trillion by 2030 and reduce global livestock production by almost eight per cent.
According to Jonathan Wadsworth, lead agriculture specialist at the World Bank Group, antimicrobial resistance will negatively affect Sustainable Development Goals such as those that focus on poverty, good health and well-being.
“Reducing the use of antimicrobials … can make a huge difference.”
Jimmy Smith, International Livestock Research Institute (ILRI)
“The money cost is too high, which can result in people’s lives being put on hold,” Wadsworth explained, citing an antibiotic in the United States for treating intestinal infections that costs US$500 for only 20 pills. “This shows that many people have no access to the medicines they may need.”
Phan Thi Van, director, Research Institute for Aquaculture, Vietnam, added, “The developing world has a high risk of antimicrobial resistance because it has the greatest demand for food production, with a rapidly growing population.”
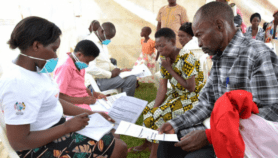
According to the meeting held in Kenya last month (21-22 February) to launch the CGIAR Antimicrobial Resistance Hub, even low level of antimicrobial resistance could drive about eight million people into extreme poverty by 2030.
“Reducing the use of antimicrobials … can make a huge difference”, says Jimmy Smith, director-general, International Livestock Research Institute (ILRI). Smith added that the hub will create partnerships and make evidence the heart of policymaking in low- and middle-income countries.
The optimal solution for addressing the antimicrobial resistance challenge is having practical research solutions appropriate for and effectively applied in low-and middle-income countries, Smith explained.
The meeting was convened by Kenya-headquartered International Livestock Research Institute (ILRI) in partnership with CGIAR — a global partnership that unites organisations engaged in research for a food-secured future.
The main aim of the hub, which is being funded by several CGIAR partners, is to support the efforts of low-and middle-income countries to tackle antimicrobial resistance as is being done in high income countries such as Denmark, the Netherlands and Sweden.According to the meeting, the CGIAR antimicrobial resistance strategy focuses on five pillars on research and interventions such as understanding knowledge, attitude, practices and incentives for antimicrobial; designing and evaluating interventions and incentives to reduce and more effectively use antimicrobial in agriculture in low- and middle-income countries.
The others pillars are capacity development and supporting evidence-based policy dialogue for studying and developing strategies to address antimicrobial resistance.
This piece was produced by SciDev.Net’s Sub-Saharan Africa English desk.