By: Bernard Appiah
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Antimicrobial resistance is a threat to Africa, but little is being done to fight it, writes Bernard Appiah.
Think of this gloomy statistic — by 2050 antimicrobial resistance (AMR) could lead to deaths of 4.15 million people in Africa every year. [1] The only continent that will overtake Africa is Asia, which could see 4.73 million people die from this canker over the same period.
But despite the potential impact of AMR in Africa, evidence suggests that not much is being done to fight it.
Just take the case of multi-drug resistant TB as a special case of AMR. According to the 2014 WHO global surveillance and response report, surveys carried out every three to five years is ideal for resource-limited settings where weak laboratory capacity could undermine the ability to carry out drug testing. [2]
“Tacking antimicrobial resistance in the health sector without focusing on agriculture is a disaster.”
Bernard Appiah, SciDev.Net
The report notes recent surveys worldwide in tracking multi-drug resistant TB in countries such as Lesotho, Nigeria, Rwanda, Senegal, South Africa and Uganda. But it adds: “Central and Francophone Africa remain the parts of the world where drug resistance surveillance data are most lacking, largely as a result of weak laboratory infrastructure.” [2]
Evidence from Ghana
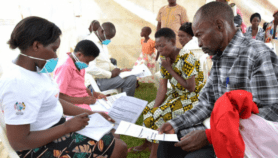
On 18-20 March this year, Ghana hosted the African Conference on Antibiotic Use and Resistance. Alexander Dodoo, the chairperson of the conference’s opening session, tells SciDev.Net that African governments need to invest in improving surveillance of AMR.
“The threat is with us and if nothing is done, it could make matters worse,” says Dodoo, who is also the director of Ghana-based WHO Collaborating Centre for Advocacy and Training in Pharmacovigilance.
Perhaps, three studies on Ghana’s antibiotic use that were briefly discussed in the communiqué issued at the end of the conference could be a wake-up call for the country and others in the sub-region.
According to the communiqué, in one study, researchers evaluated prescriptions of 2,660 patients and found that about half of them received antibiotics. Only 20 per cent of the prescribers were physicians, with most prescribers being nurses and medical assistants.
The report notes that in another study, which involved interviews of patients and physicians, researchers found that doctors had little time for each patient. “Physicians prescribe antibiotics without clinical examination, microbiological sampling, instructions or information about indications or disease,” the report adds.
Widespread prescription of antibiotics without rigorous clinical testing is a fuel for driving resistance of these medicines.
In a third study, researchers tested urine and blood samples of community dwellers for ten antibiotics. They also tested samples of chicken meat, river water and irrigation water for the same antibiotics.
The report adds: “Up to 70 per cent of community dwellers, who denied having taken antibiotics in the previous 14 days had at least one antibiotic found in their urine. Antibiotic residues were found in chicken meat, river water and water used for irrigation.”
“Antimicrobial use in communities could also be tackled if school children are used as agents of change.”
Bernard Appiah, SciDev.Net
Were the community dwellers lying? Did the antibiotics get into their urine through agriculture? As health researchers search for solutions to antimicrobial resistance, it is important they also look beyond non-health institutions.
One health approach
Antimicrobial resistance is a classic issue that illustrates one health, a concept that values the integrative relationship between human and animal health. Tacking antimicrobial resistance in the health sector without focusing on agriculture is a disaster.
Unfortunately, just as studies on the subject in human populations are lacking on the continent, so are those that focus on agriculture. For example, a report by the International Livestock Research Institute published last month shows a need to invest in conducting research on AMR in developing countries. [3]
“While AMR pathogens in animals and their products undoubtedly contribute to AMR infections in people, the literature from developing countries is insufficient to draw firm conclusions on the extent of this contribution,” says the report. “We don't have accurate information on antibiotic use in developing countriesbut agricultural use probably exceeds medical use; most use is probably in intensive production systems; and, use is probably increasing rapidly.”
The report identifies Brazil, China and India as hotspots of increasing antimicrobial use based on livestock intensification patterns, but cites other countries including Nigeria as future hotspots.
Tacking the menace will require strengthening of weak laboratory infrastructures, strong regulatory environments and support for researchers to conduct surveillance and community-based studies on the subject. But interventions that promote behavioural change among the general population should not be ignored in the fight against AMR.
Involving media and children
In Ghana, a project led by the Ministry of Health to improve advocacy on antimicrobial resistance has actively involved media professionals. The project aimed to empower the media in Accra to help them report on the subject.[4]
Antimicrobial use in communities could also be tackled if school children are used as agents of change. For example, in Africa antibiotics may be put into the sores of children to aid their healing. If a child knows that such a practice could contribute to antimicrobial resistance, they are likely to educate their parents against this practice.Nothing could be more embarrassing to an adult than a child say, “Mommy, I am told that what you are doing is wrong.”
Clearly, the fight against antimicrobial resistance in Africa requires culturally relevant interventions, including those involving policymakers.
Let’s not pretend that antimicrobialresistance is not in Africa because of lack of data. The time to get serious aboutfighting antimicrobial resistance is now.
Bernard Appiah is regional subeditor of SciDev.Net’s Sub-Saharan Africa edition
This article has been produced by SciDev.Net's Sub-Saharan Africa desk.
References
1. Jim O’Neill andreview committee members Antimicrobial resistance: Tackling a crisis for thehealth and wealth of Nations (Review committee set up by the UK Government, December 2014)
2. WHO Global tuberculosis report(WHO, 2014)
3. Antibiotic drug use, monitoring of resistance (ADMER) project Communiqué: African conference on antibiotic use and resistance, 18-20 March 2015 (ADMER project, 2015)
4. Delia Grace Review of evidence on antimicrobial resistance and animal agriculture in developing countries(ILRI, June 2015)
5. Isaac Kofi DzokpoJournalists urged to use platforms to educate public on antibiotics misuse(spyGhana.com, 25 April 2015)