Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
HIV, the fastest mutating organism, now poses the threat of a second drug-resistant epidemic.
On 1 December 2011, President Obama declared that we now have the tools for an 'AIDS-free generation'.
Made just over 30 years after HIV was discovered, this declaration was a stunning turnaround in the fight against HIV and AIDS. The world had come together to fight a scourge that had killed over 30 million people and transformed it into a manageable, chronic illness. Persons infected with HIV were now referred to as “people living with HIV (PLHIV),” highlighting that HIV is not only a survivable disease but also one where normal life is possible.
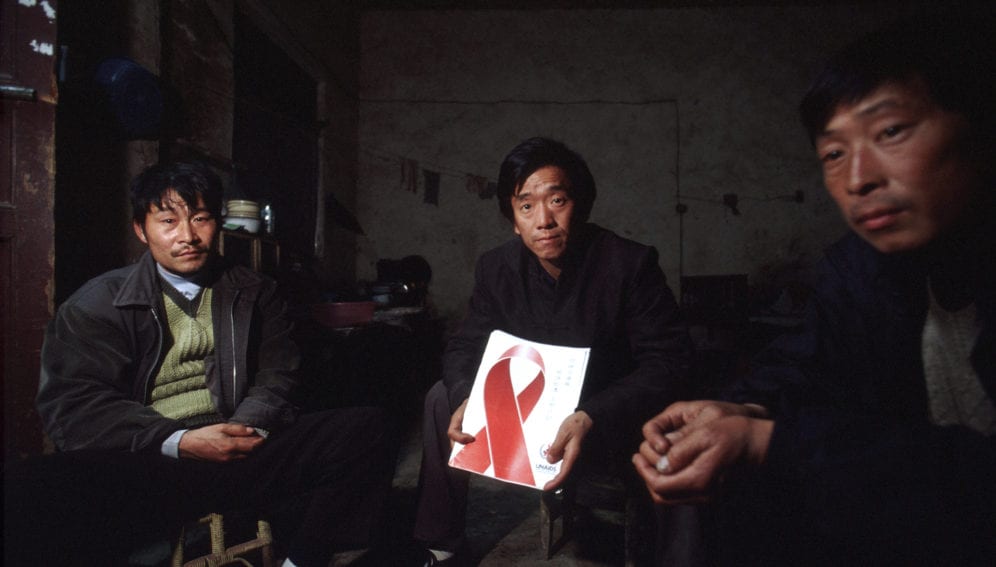
While this rosy picture of HIV elimination may be achievable in theory, the reality is far more depressing. As the world gathers in Amsterdam this 23-27 July for the AIDS 2018 conference, a long shadow hangs over the celebration. In the bleak light of a rapid increase in HIV drug resistance, in the poorest parts of the world, it appears that a second drug-resistant HIV epidemic is on the horizon.
“In the bleak light of a rapid increase in HIV drug resistance, in the poorest parts of the world, it appears that a second drug-resistant HIV epidemic is on the horizon”
Edsel Maurice Salvana, Philippine National Institutes of Health
Progress in the treatment of HIV and AIDS has indeed been positive. Anti-retrovirals (ARVs), when started early, can restore PLHIV’s life expectancy. The massive worldwide rollout of ARVs has saved millions of lives. Generic ARVs now cost less than a dollar a day, and an aggressive global push to put as many PLHIV on ARVs has been quite successful. HIV cases have dropped worldwide by more than 30 per cent since 2000 and deaths have declined by over 40 per cent since 2003. In sub-Saharan Africa, most countries have seen a 25—50 per cent drop in cases in the last decade.
But concomitant to this success is an alarming jump in drug-resistant HIVs.
HIV – fastest mutating organism
HIV is the fastest mutating organism on the planet, being 1 million times faster than bacteria. The retrovirus uses ribonucleic acid (RNA) to reproduce, in contrast to the DNA that humans and most organisms use. To infect a human cell, HIV converts its RNA into DNA using an enzyme called reverse transcriptase. Unlike our own human enzyme DNA polymerase which faithfully copies DNA when our cells reproduce, reverse transcriptase is like a faulty photocopying machine that makes frequent mistakes. In addition, HIV has two complete sets of genes. When two different HIV strains infect the same host cell, they can “mate” and recombine their genetic material, giving rise to new kinds of recombinant viruses.
HIV is a zoonotic virus, or an animal virus that jumped to humans. Based on analysis of its genetic material, it made the jump from apes to humans at least five times. Over 90 per cent of HIV in the world is part of the so-called HIV-1 Group M, which was transmitted to humans from chimpanzees.
Because of HIV’s prodigious rates of mutation, Group M has evolved into genetically diverse subtypes, each of which differs by 25—35 per cent of its total genetic material. To put this into perspective, the genetic diversity of the entire human race from the proverbial Adam to the billions of people alive today is less than 0.1 per cent.
HIV-1 Group M has nine distinct subtypes: A, B, C, D, F, G, H, J and K. What happened to E and I? It turns out these two are made up of combinations of subtypes, giving rise to a new kind of virus known as a circulating recombinant form, or CRF. The old subtype E is now known as CRF01_AE, the very first recombinant subtype or literally an “offspring” virus of two subtypes. There are now nearly 100 CRFs, some of which are recombinants of the CRFs, further contributing to the unprecedented genetic diversity of HIV.
The most studied HIV subtype is B, which is the predominant strain in the US and Western Europe. While it accounts for only 12 per cent of HIV cases worldwide, most research on treatment is based on subtype B. We have been dangerously assuming that treatment that works for this subtype is just as effective for other subtypes, despite the large genetic difference between them. Some of these less-studied, non-B subtypes seem to respond differently to treatment, progress to AIDS faster, and develop drug resistance faster.
As HIV mutates, fast proper treatment typically requires a combination of three drugs. Poor adherence or using a suboptimal regimen results in resistance. Even in the best of circumstances treatment can fail, and drug-resistant virus may be transmitted. As drug resistance increases in a community, second-line ARVs need to be available to continue proper treatment. The more ARVs available, the more choices there are for effective treatment.
Currently, there are 28 approved ARVs in the US, but only six or less of these are available in most parts of the world. Therefore, PLHIV in resource-poor settings who fail first-line treatment may have one second-line regimen at most. If they become resistant to this last-line treatment, they progress to AIDS and die.
In 2015, WHO revised its HIV treatment guidelines and recommended a one-pill, once a day ARV combination as the preferred first-line treatment for HIV worldwide. This combination – tenofovir, lamivudine (or emtricitabine), and efavirenz – was hailed as an excellent strategy for quickly rolling out ARVs globally.
In contrast, later that year, the US guidelines no longer recommended the WHO regimen for first-line treatment due to increasing drug resistance and side-effects. In 2016, a WHO meta-analysis comparing one of the US-recommended first-line ARV agent dolutegravir to efavirenz and lopinavir/ritonavir (a common second-line agent used in developing countries) showed the inferiority of both efavirenz and lopinavir/ritonavir.
In June 2017, WHO released its latest global HIV resistance report based on countrywide surveys. It looked at both acquired drug resistance (ADR) or resistance that develops on treatment and transmitted drug resistance (TDR) or resistance that is already present in the virus prior to starting ARVs. The report showed that up to 30 per cent of PLHIVs failed treatment due to ADR at one year in countries like Cameroon. It also showed that TDR to efavirenz was as high as 20 per cent in countries like Nicaragua. Across the board, from Africa, Asia and Latin America, ADR, and TDR was on the rise.
Increasing drug-resistance trend
These facts paint a picture that first-line ARVs as recommended by WHO may no longer be adequate to address the increasing trend of drug resistance and a push for newer and more potent agents is in order. This is almost certainly just the tip of the iceberg since ARV rollout worldwide was geared towards starting as many PLHIV on ARVs as soon as possible. Unfortunately, proper monitoring of emerging drug resistance is highly technical and may be beyond the capabilities of low-income countries.
The Philippines has the fastest growing HIV epidemic in the world. One factor that stands out in this epidemic is the shift of the predominant HIV subtype from B to CRF01_AE. We are seeing increasing rates of resistance, both transmitted and acquired, along with unusual resistance patterns especially to tenofovir, a mainstay of HIV and hepatitis B treatment. We are also seeing recombinants of B and CRF01_AE.
To be clear, CRF01_AE is not a new strain, but we know very little about its behaviour and response to treatment. We urgently need more research on CRFs and non-B subtype viruses to address the encroachment of these viruses into other countries, which may trigger a similar secondary epidemic.
In conclusion, it can no longer be “business as usual” for WHO, UNAIDS, and other stakeholders in HIV. Certainly, we should be proud of the tremendous progress that the world has made in curbing the HIV pandemic. But the virus is by no means defeated and continues to evolve. It continues to defeat efforts for a durable cure or a vaccine. There are myriad signs of an encore.Perhaps it will not be as immediately apparent in developed countries where new, potent agents are plentiful. But as it was in the 1980s when millions had already died in Africa before the world took notice – and only when the deaths reached the shores of America – this HIV 2.0 will start in the poorest countries with little capacity to handle the problem and eventually make its way to the countries that are best equipped to handle it, and the cycle starts anew.
We need to nip this in the bud. It is not acceptable that the WHO with its Western-centric consultants continues to insist that all HIV subtypes respond equally well to treatment in the face of the increasing evidence of ADR and TDR. It is not acceptable that they insist that the world continue to use WHO-recommended regimens when those have been abandoned in their own countries. It is not acceptable that cost and for-profit considerations remain a barrier for providing more effective ARVs in resource-limited settings, when developing countries are the ones who can least afford them and are most vulnerable to another HIV pandemic. We need to rekindle the old flame of the early HIV activists who would not take no for an answer, and demand that we do what needs to be done to save lives.
After all, as AIDS activists, it’s in our DNA.
Dr. Edsel Maurice Salvana is the director of Molecular Biology and Biotechnology at the Philippine National Institutes of Health. He is an infectious disease physician and a staunch advocate for proper treatment of HIV and is pushing for urgent action on the dangerous increase in drug-resistant HIV.
This piece was produced by SciDev.Net’s Asia & Pacific desk.