By: Neena Bhandari
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[SYDNEY] Genetically-intact HIV hides in the same cells of the human immune system that are supposed to attack and destroy pathogens, scientists at Westmead Institute for Medical Research, Sydney University, discover in a new study.
Previously, it was thought that HIV hides primarily in central memory T-cells during effective anti-HIV therapy. But, in the study published this month (19 October) in Cell Reports, the scientists show that replication-competent HIV persists in specific subsets of CD4+ immune memory T-cells.
“It will allow us to identify the cells which contain infectious, replication-competent virus, opening up promising possibilities for targeting this remaining virus for elimination from the body”
Sarah Palmer, Sydney University
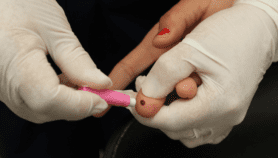
HIV infects white blood cells known as T lymphocytes, particularly the CD4+ T cells that recognise infection and gets the immune system to respond. Following HIV infection, if anti-HIV therapy is not initiated, the number of CD4+ T cells in the blood begin to fall, though the process may be slow.
Sarah Palmer, associate professor at Sydney University, whose team developed a full-length genetic sequencing assay for HIV says: “This assay identifies where and determines how much replication-competent virus remains in the CD4+ T cells of an HIV-infected individual even after years of effective anti-HIV therapy."
"It will allow us to identify the cells which contain infectious, replication-competent virus, opening up promising possibilities for targeting this remaining virus for elimination from the body,” she adds.
The researchers will now conduct studies to determine how long replication-competent viruses persist in these specific cells during anti-HIV therapy and identify cellular markers unique to these cells so they can be targeted by treatment strategies.
“Therapies can now be directed towards the specific cells containing this genetically intact virus. This new treatment strategy could be in the form of nanoparticles, which deliver therapies directly to cells containing the infectious, replication-competent virus,” Palmer tells SciDev.Net.
Only about five per cent of HIV is genetically intact and it hides in the effector memory T-cells while the rest act as a decoy and divert attention away from the “real” virus, the study says.
“The immune system cannot discern replication-competent virus from defective virus. Some defective viruses can produce viral proteins which are recognised by the immune system and then the cells containing the defective virus are eliminated. But, because there is so much more defective virus in the cells than genetically intact virus, these defective viruses act as a decoy and divert the immune system,” explains Palmer.
As many as 36.7 million people globally were living with HIV in 2016. There is still no vaccine against HIV which is known to cause acquired immune deficiency syndrome (AIDS).
“Today we have excellent HIV treatments which can keep most people well by driving down HIV in the body to “undetectable” levels,” says Cipriano Martinez, president, National Association of People with HIV, Australia. “But, even with these treatments, HIV are still able to hide in various cells of the body and cannot be completely eliminated.”“This research is timely and provides new information to assist in the development of therapies aimed at fully eliminating HIV from the body,” says Martinez.
This piece was produced by SciDev.Net’s Asia & Pacific desk.