By: Lyndal Rowlands
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Timor-Leste, a young nation with a rapidly growing population, is facing new challenges in its healthcare system as it move towards maturity, many of which can be addressed by an increased focus on evidence-based medicine.
The small island nation voted for independence from Indonesia in 1999 and over the past 15 years has had to rebuild in many areas including health and education. An agreement with Cuba to rapidly scale up the number of Timorese doctors has seen a four-fold increase in the number of Timorese doctors from 2011 to present. The new junior doctors are expected to help fill the gap left behind by Indonesia. In the past, most doctors and other professionals in Timor-Leste were from Indonesia. Since independence, this gap has been temporarily filled by international doctors, mostly from the Cuban Medical Brigade.
The expected addition of over 1,000 new junior doctors to Timor-Leste’s health system between 2011 and 2017 presents new challenges and opportunities for clinical training. These include establishing Timor-Leste’s national hospital as a teaching hospital, preparing junior doctors to work independently in often isolated rural clinics and teaching evidence-based medical practice within the constraints of a low resource setting.
Ongoing problems for healthcare in Timor-Leste include limited laboratory technology and imaging, especially outside of the national capital Dili, and limited access to medicines. The Ministry of Health reported in 2010 that as many as 64 per cent of hospital admissions did not have a diagnosis on discharge.
Evidence-based healthcare
Evidence-based medicine involves using the best and most up-to-date information available to make decisions about patient care.
A study published in PLOS Medicine by its global health editor Paul Chinnock and his colleagues describes the rationale for evidence-based medicine as follows: “Wherever healthcare is provided and used, it is essential to know which interventions work, which does not work, and which are likely to be harmful.”
Chinnock’s study argues that evidence-based medicine is even more essential to the developing world than it is to the developed world but real limitations remain, including access to relevant systematic reviews of the effectiveness of healthcare interventions originating from developing countries.
With the first new graduate doctors returning from Cuba, the national hospital has begun to show signs of working as a teaching hospital, with junior doctors learning and participating in evidence-based medicine through ward rounds, tutorials, lectures and audits. Clinical training has primarily been delivered by the Cuban Medical Brigade and the Australia Timor-Leste Program for Assistance for Secondary Services funded by the Australian government, as well as a small number of Timorese specialist doctors.
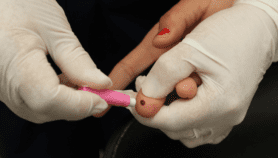
For example, in the paediatric department at the national hospital, clinical training has helped junior doctors learn how to make accurate diagnoses on the basis of history, clinical examination, X-rays and laboratory findings. This has discouraged the practice of polypharmacy or the use of multiple medications by a patient, and is helping doctors to correctly diagnose conditions such as acute bronchiolitis that can be misdiagnosed as bronchopneumonia. Junior doctors participating in clinical training are encouraged to review and learn from difficult cases, and to present them to other doctors at audit meetings and grand rounds, the lunchtime lectures open to all clinical staff.
Online resources are also helping with the move towards evidence-based medicine. They include UpToDate and the WHO’s HINARI project. Open access to resources such as HINARI helps doctors in developing countries to use the most recent available literature to support clinical decision-making. Yet this is made more difficult by Timor-Leste’s slow and expensive internet, which lags behind much of the developing world.
Generating internal health research
Nobel Peace Prize winner and former Timor-Leste President José Ramos Horta recently called for greater investment in health, highlighting the potential for neighbouring countries such as Australia to contribute to health research in Timor-Leste through its research institutions.
More contributions from Timor-Leste to research will help complete the evidence-based medicine cycle by providing relevant information to inform clinical decision making. Notable contributions include publications from Timorese academics Nelson Martins and Joao Martins.
However, many of the published articles on health in Timor-Leste until now have been descriptive studies, usually based on questionnaires or surveys. This means Timor-Leste has contributed little evidence-based medicine. Although much of international evidence-based medicine can still be applied to clinical practice in Timor-Leste, it is now a research challenge for Timor-Leste to carry out high quality research and contribute to EBM.
In the short term, Timor-Leste needs to prioritise clinical training for the hundreds of recently graduated junior doctors, encouraging them to use the best evidence-based medicine available in their everyday practice.
Lyndal Rowlands is Monitoring and Evaluation Officer for the Royal Australasian College of Surgeons in Timor-Leste. She can be contacted at [email protected] and LinkedIn.
This article has been produced by SciDev.Net's South-East Asia & Pacific desk.
References
Augustine Asante and others Retaining doctors in rural Timor-Leste: A critical appraisal of the opportunities and challenges (World Health Organization Bulletin, Volume 92, April 2014)
David Brewster Avoiding polypharmacy and therapeutic nihilism in medical training in poor countries (Medical Education, Volume 48, January 2014)
J. Cabral and others Scaling-up the medical workforce in Timor-Leste: Challenges of a great leap forward (Social Science & Medicine, Volume 96, November 2013)
Jose Ramos-Horta Aid-for-trade program not what the doctor ordered (The Sydney Morning Herald, 13 May 2014)
Paul Chinnock and others Is evidence-based medicine relevant to the developing world? (PLOS Medicine, May 2005)