By: Neena Bhandari
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
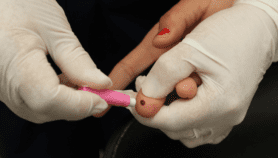
[SYDNEY] Rural women in low-income households cannot access healthcare services due to distance and financial reasons. However, overall, healthcare access has improved in 27 countries of the Asia Pacific region over the past decade, says a new joint report by the Organisation for Economic Co-operation and Development (OECD) and the World Health Organization (WHO).
Health at a Glance Asia-Pacific 2018 notes that in Nepal and the Solomon Islands, about three in four women with the lowest household income reported difficulties in accessing healthcare due to financial reasons; two in three reported having unmet care needs due to distance.
The report highlights that achieving Universal Health Coverage and the Sustainable Development Goals (SDGs) is based on the “leave no one behind” premise.
“By measuring the poverty of individuals, we can see where inequality exists within households and better understand how gender, age, disability and geography affect opportunities and outcomes.”
Joanne Crawford, International Women’s Development Agency
Mark Landry of the Department of Health Systems Development, WHO regional office for South-East Asia, tells SciDev.Net, “This also means leave no disaggregated data behind in order to measure and monitor within country health inequalities and set policy– and target-effective interventions according to the evidence.”
Over the past year, many countries have begun toanalyse and interpret disaggregated data stratified by multiple equity dimensions to better inform decision making.
While infant and maternal mortality rates across the lower-middle and low-income Asia Pacific countries have reduced since 2000, the average of 30 deaths per 1,000 live births in these countries is still eight times that for the 36-member countries of OECD. Furthermore, maternal mortality rates are twice the SDGs’ target of 70 deaths per 100,000 live births, according to the report.
Joanne Crawford at the International Women’s Development Agency tells SciDev.Net: “Individual-level measurement of multidimensional poverty — such as the individual deprivation measure — can provide a powerful complement to existing data such as in this report. By measuring the poverty of individuals, we can see where inequality exists within households and better understand how gender, age, disability and geography affect opportunities and outcomes.”
The report notes an increase in out-of-pocket expenditure on health goods and services in lower-middle and low-income countries. On average, household out-of-pocket expenditure accounted for 48.2per cent of total health expenditure, with spending on pharmaceuticals accounting for almost one-third of all health expenditure in these countries in 2015.
“There is a greater need to increase public spending and expand social health insurance programmes,” Stephen Jan, head of the Health Economics and Process Evaluation Programme at the George Institute for Global Health in Sydney, tells SciDev.Net.The lower-middle and low-income countries spend under US$200 per person per year on health, against US$670 in upper middle-income and US$3,450 in high-income countries.
“Policies to improve access to care for poor people and disadvantaged groups need to tackle not only affordability but also effective access to services. [This can be done] by promoting an adequate supply and distribution of health workers and services throughout the country,” Luca Lorenzoni, policy analyst at the health division of OECD, tells SciDev.Net.
Disparities in the use of essential services — such as access to antenatal care and immunisation of children — based on income and education remain large, Landry says. “Interventions to improve health literacy among excluded groups, including those in remote and underserved areas, merit greater attention.”
This piece was produced by SciDev.Net’s Asia & Pacific desk.