Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Collaboration between public health systems and communities is crucial to containing dengue viral fever in South Asia, writes Nalaka Gunawardene.
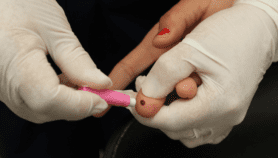
There is no direct treatment for dengue and no fully effective vaccine as yet. But early detection and proper caring for symptoms — which include fever, rash, muscle pain and damage to the blood vessels — can keep death rates low.
For now, the best control strategy involves destroying the tenacious vectors and protecting against their bites. These can succeed only if everyone joins the effort. We are as strong as the weakest link.
Dengue is mostly transmitted by a mosquito species named Aedes aegypti, which breeds in water containers in and around homes. It is thus closely linked to environmental factors and human behaviour.
Now the world's most rapidly spreading vector-borne viral disease, dengue has recorded a 30-fold increase over the last 50 years, according to the World Health Organisation (WHO). [1]
The disease is not new. For much of history, however, dengue was confined to a few tropical places. It was only in the last century that the dengue mosquito spread widely with increased human travel and movement of goods.
More than 2.5 billion people – over 40 per cent of the world’s population – are believed to be at risk from dengue today. WHO estimates that there are some 50 to 100 million infections worldwide every year. [1] Other researchers have put the annual figure at 390 million, indicating a vast number of unreported or misclassified cases. [2]
Everyone agrees, though, that dengue is on the rise. Three-quarters of those affected by dengue live in the Asia Pacific. In many countries, dengue causes heavy economic and social burdens.
Monsoonal sting
As it spreads, dengue is challenging policy makers and public health systems to rethink strategies to cope with the disease and its vector.
In recent years, South Asian countries have seen a hike in dengue cases towards the end of the mid-year summer monsoon. This year, in particular, India has experienced an upsurge in dengue cases and deaths, triggering public and media outcry.
As Patralekha Chatterjee, an Indian journalist specialising in health and urban issues, wrote: “This is among the worst dengue outbreaks in recent times, but the big picture is monotonously familiar. Every monsoon there are outbreaks of all sorts of mosquito-borne and other infectious diseases…but each time we act as if the disease has crept in stealthily, whereas we all know why it has happened and what needed to be done to prevent it.” [3]
Effective prevention and clinical management of infectious diseases require good leadership at local government level. Chatterjee cites the example of Surat, a coastal industrial city of five million people in Gujarat state. After an outbreak of plague in 1994 that killed over 50 residents and drove thousands away, the city officials completely revamped their public health and environmental management systems.
Today, Surat employs a network of around 500 health and surveillance workers who routinely check on people, administer medicines and collect data that help health officials see outbreaks before they are reported in hospitals.
Once every fortnight, they visit every home in the city checking for malaria, dengue, chikungunya and filariasis. This routine happens round the year (unlike other municipalities that start surveillance only when there is an outbreak). [4]
Complicating India’s dengue problem is the lack of comprehensive and reliable data. From 2006 to 2012, the nation of 1.2 billion has reported an annual average of 20,474 dengue cases – which seems suspiciously low. Last year, a group of Indian and US researchers estimated that actually some 5.8 million Indians suffer from dengue every year – which is 282 times higher than the official figure.
The researchers, led by Donald Shepard of Brandeis University, also calculated that India was spending around US$ 550 million annually on dengue medical care. Factoring economic and productivity losses, they reckon that dengue costs India more than US$ one billion each year. [5]
Silent Disaster
India is not alone in underestimating dengue’s spread and impacts. Beyond seasonal spikes, dengue often escapes the sustained attention of policy makers, donors and media in many other countries.
For this reason, the International Federation of Red Cross and Red Crescent Societies (IFRC) has called it one of the world’s silent disasters.
“It has catastrophic consequences for the individuals, families and communities affected. A long-term strategy covering effective vector control, access to health services and early clinical management are steps towards ensuring that people are no longer abandoned to unnecessary, silent suffering caused by the disease,” IFRC said in a 2013 report. [6]
Ground level interventions to control dengue need to be backed by on-going research. This is because the virus and vector keep adapting fast.
For example, dengue was long considered an ‘urban’ disease, thriving in crowded, poorly managed cities and towns. But recent research in India and Sri Lanka suggests the disease is fast spreading to rural areas as well.
Two Lankan researchers, using official epidemiological data, show in a recent analysis how there has been a ‘dramatic increase’ in dengue in all other provinces besides the most urbanised Western Province of Sri Lanka.
P. D. N. N. Sirisena and F. Noordeen of the University of Peradeniya found that Sri Lanka’s dengue coverage map keeps expanding each year. After the war ended in mid-2009, dengue has become endemic in the former war areas of Northern and Eastern Provinces. They attribute this to the freer movement of people on the island. [7]
Climate Factor
Could climate change also cause or add to this rise?
Very likely, say Sirisena and Noordeen. The recent extended rainy seasons in Sri Lanka — with heavy rains and floods — could be one reason for dengue becoming both rampant and more unmanageable (total cases in 2014 were 47,500, a sevenfold increase since 2008). [8]
The dengue mosquitoes multiply fast when there is more rainfall, higher temperatures and poor drainage that leads to more stagnant water.
Well-kept households and cities can deprive them of the watery medium to breed. Proper disposal of municipal waste should also be part of control strategies.
In a rapidly urbanising and climate stressed world, dengue is yet another test of our collective resilience. As Surat has shown, public health needs to be everybody’s business.
Nalaka Gunawardene is a Colombo-based science writer, blogger and development communication consultant.
This article has been produced by SciDev.Net's South Asia desk.
References
[1] Vector borne diseases: dengue. WHO Media Centre.
[2] The global distribution and burden of dengue. Nature. 25 April 2013
[3] Smart cities need smart healthcare. By Patralekha Chatterjee. Asian Age. 23 September 2015.
[4] How Surat became India’s public health leader. By Patralekha Chatterjee. Cityscope.org. 5 June 2015.
[5] Economic and Disease Burden of Dengue Illness in India. D S Shepard, et al. American Journal of Tropical Medicine and Hygiene. 6 October 2014.
[6] Dengue: Turning up the volume on a silent disaster. IFRC. 2013.
[7] Evolution of dengue in Sri Lanka — changes in the virus, vector, and climate. P.D.N.N. Sirisena, F. Noordeen. International Journal of Infectious Diseases. February 2014.
[8] Climate change and dengue in Sri Lanka. by Amantha Perera. SciDev.Net. 12 September 2015.