Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Consider what you would do if you or a loved one gets sick. Would it be difficult to get the healthcare you need or worry about how you will pay for it?
Healthcare shouldn’t be a privilege of the wealthiest few. It is an integral part of our daily lives and our future plans and that is why health is considered a basic human right.
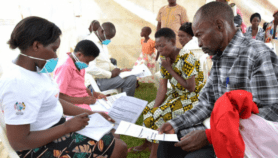
I travelled to Nairobi, Kenya, in April to talk about universal health coverage — the idea that all people can have access to quality health care, without financial hardship.
While Kenya has seen improvements in areas such as HIV care and treatment and child survival, many Kenyans still struggle to access basic healthcare. Health facilities are too few, and often understaffed. Where facilities are available, cost is often a burden.
“Healthcare shouldn’t be a privilege of the wealthiest few. It is an integral part of our daily lives and our future plans and that is why health is considered a basic human right.”
Jonathan D. Quick, Management Sciences for Health (MSH).
Today, close to 50 per cent of health spending in Kenya comes straight from patients’ pockets, with Kenyans spending about 10 per cent of their budgets on healthcare. [1] That’s high for a country with Kenya’s resources, and high compared to a regional average of closer to 30 per cent out-of-pocket spending.
If you’re one of the lucky few, you have health insurance that will help cover the cost of care. If not, getting sick could mean losing your savings and going into debt. Lack of a safety net hurts everyone, and it places the greatest burden on the poor. These challenges aren’t new and they are not unique to Kenya or other African countries. Even in the United States, where I live, people continue to struggle with healthcare access. Every country could be doing better.
Turning point in Kenya
The national government in Kenya has committed to tripling the share of its budget devoted to health to 15 per cent — and, more importantly, to providing free primary healthcare for all Kenyans, with a focus on the most vulnerable populations. The National Health Policy of Kenya sets forth strategies supporting a universal health coverage agenda, in line with the country’s long term development agenda of Vision 2030. These plans support the right to health as provided for in Kenya’s 2010 constitution.
Several changes are already under way. Last year, maternity fees were waived at public facilities, and user fees previously charged in dispensaries and health clinics were eliminated. These steps show political commitment and are improving access to primary care for many Kenyans.
What Kenya and many other African countries need now is to harness widespread demand for better health care and mobilise health leaders at national and county levels to begin extending access to more people.
The concept of universal health coverage has received a strong endorsement from the World Health Organization and other key players. It has gained momentum globally to be included in the international development agenda when the Millennium Development Goals — a set of goals and targets agreed to globally in 2000 — expire in 2015.
Transform healthcare
At Management Sciences for Health (MSH), a non-governmental organisation that works in more than 60 countries, we believe universal health coverage is the only approach for transforming health systems to provide everyone all the services they need.
“What Kenya and many other African countries need now is to harness widespread demand for better health care and mobilise health leaders at national and county levels to begin extending access to more people.”
Jonathan D. Quick, Management Sciences for Health (MSH).
This may sound like a lofty idea, but we know it can be done. Many countries — at all levels of economic development — have taken meaningful steps towards broader, more equitable coverage, making health care more available and affordable for millions of people.
Around the world, Mexico, Thailand and Turkey and others have shown that universal coverage is not just a privilege for the richest countries. There are great examples from Africa too. Ninety-eight per cent of Rwandans, for instance, have health coverage.[2] This means almost everyone, even the poorest members of society, can walk into a clinic and receive care. Those who can afford to, pay annual premiums; the poor are sponsored by the government.
Rwandans pay a small charge to providers when they receive health services, reinforcing shared responsibility without putting health care out of reach. Reforms aimed at expanding health coverage are being implemented in other countries too, such as Ghana and Mali.
MSH is doing its part to promote better health throughout Africa and the world. In Kenya, we lead five projects in the health sector to develop leadership, organisational and financial capacity, improve access to pharmaceuticals and health commodities, and build the capacity of laboratory systems with support from the US Agency for International Development.
Each of these projects is strengthening the health system’s ability to deliver better health coverage. MSH, with support from the Rockefeller Foundation, has also been operating the Health for All campaign, which advocates for universal health coverage in Ethiopia, Kenya and Nigeria.
For the past two years, the campaign has been mobilising communities and health leaders to ensure access to health care — building awareness at national and local levels; and ensuring that issues such as infrastructure, health workers and financing receive adequate attention in the planning process.
I hope the people of these countries and others will engage in the conversation, lending their voices to the chorus of those calling for wider healthcare access. Too many people still face financial and other barriers to accessing essential health services. Now is the time for a lasting commitment to universal health coverage in Kenya and throughout Africa.
Jonathan D. Quick, a family physician and health management specialist, is president and CEO of Management Sciences for Health (MSH). An international non-profit organisation with teams in Africa, Asia, and Latin America, MSH builds local capacity to achieve greater health impact through stronger health systems. He can be contacted at [email protected]
This article has been produced by SciDev.Net's Sub-Saharan Africa desk.
References
[1] BMC Health Services Research doi:10.1186/1472-6963-12-413 (2012)
[2] McNeil, D.G. Rwanda’s health care success story (New York Times, 2013)