By: Carol Campbell
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Inadequacies in HIV testing and treatment of pregnant women in South Africa means mother-to-child transmission is largely going unchecked in local clinics and hospitals, new research has found.
The study was published in Aids Research and Therapy last month (November).
Prevention of mother-to-child transmission programmes (PMTCT) are a standard protocol in South Africa. HIV-positive women take a dose of the antiretroviral drug nevirapine before delivery and the baby is given a dose within 72 hours of birth.
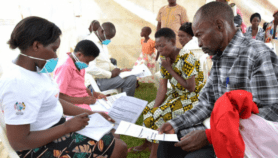
The researchers interviewed 58 women about their antenatal care at centres in the country’s KwaZulu Natal, Eastern Cape and Western Cape provinces.
They found that women visiting antenatal clinics are not always tested for HIV, even when they want to be, and that 15 HIV-positive mothers were not given nevirapine before they delivered — which could result in an increased risk of mother-to-child HIV transmission.
Those that missed taking nevirapine did so not because of stigma or ignorance, but because they did not know their status or were not offered the drug.
It is largely because of these failures that the country’s infant mortality rate is rising and is now 69 deaths per 1,000 births, Tanya Doherty, senior scientist at the Health Systems Research Unit at South Africa’s Medical Research Council and author of the paper, told SciDev.Net.
This means South Africa is unlikely to meet the fourth United Nations Millennium Development Goal that aims to reduce under-five mortality by two-thirds between 1990 and 2015.
"It is inexcusable that more is not being done in South Africa to save babies’ lives," she says.
"If the PMTCT programme was implemented more effectively, including routine testing of antenatal women and a dual drug regimen for women testing HIV positive, many lives could be saved."
Doherty says that dual therapy for HIV positive pregnant women involving daily doses of the anti-HIV drug AZT from 28 weeks of pregnancy, a single dose of nevirapine in labour and then a week-long AZT course for the newborn infant is now advocated by the WHO.
Co-author Lungiswa Nkonki says the responsibility for ensuring that women were given proper treatment lies with hospital management and the National Health Department. "Systems have to be in place to ensure there is follow-up at every stage of the process," she says.
Link to full paper in AIDS Research and Therapy ![]()
Reference: AIDS Research and Therapy 4 doi 10.1186/1742-6405-4-27 (2007)