Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
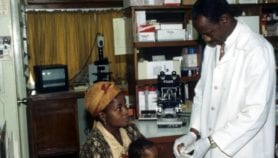
The number of clinical trials conducted in South America by multinational pharmaceutical companies is on the rise, leading to unregulated and exploitative tests, according to an article in The Nation magazine.
According to the US Food and Drug Administration, clinical trials in developing countries have grown in number by eight per cent a year since 1997. And overseas trials account for 40–65 per cent of all trials on products certified by the FDA, a 2010 report by the inspector general of the US Department of Health and Human Services (HHS) found.
But, of the 6,500 tests conducted overseas in 2008, less than one per cent were inspected by the FDA.
According to The Nation, recent coverage of US clinical trials in the developing world has focused on Africa and India — while trials in South America have "quietly spiked". The HHS report said that in 2010, Central and South America had the highest number of subjects per site — and accounted for more than a quarter of all subjects enrolled in foreign trials.
Trials in developing countries are attractive to drug developers because fewer regulations and the ease of recruiting patients allow drugs to pass from laboratory bench to pharmacy counter quickly and cheaply, says the article.
Additionally, it says, the surge in clinical trials outside of the United States is straining the FDA’s ability to regulate the process.
The article cites Peru, which conducts one of the highest number of trials in the world, as an example of how this lack of regulation leads to a drop in the quality of trials, putting patients at risk.
The country is a "paradise of human experimentation", according to Herberth Cuba, a Peruvian gynaecologist who runs the watchdog group the Peruvian Medical Association.
The targeting of poor communities in Peru is a form of "medical colonialism", he tells The Nation.
Another problem arises from the out-sourcing of ethical review services, known as institutional review boards (IRBs), to private companies, the article says.
IRBs consisting of medical professionals and community members, have the authority to stop unethical clinical trials. These boards exist to prevent ethical abuses, such as deliberately infecting Guatemalans with syphilis to study penicillin in the 1940s. However, there has been a recent rise in for-profit companies offering these services, leading to vested interests, where decisions are often made on economic, rather than ethical, grounds.
"The IRB system is vulnerable to unethical manipulation," an official from the US Government Accountability Office told a congressional committee.
References
null