By: Pauline Okoth
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
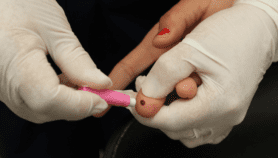
Giving the babies of HIV positive mothers preventative antiretroviral drugs slashes the risk of transmitting the virus during breastfeeding, a study has found.
The study, which monitored breastfeeding mothers with HIV, found that only 1.5 per cent of babies given such drugs got the virus during one year of feeding. Without treatment, there is a 5-20 per cent chance of passing HIV to a baby through breastfeeding, according to the World Health Organization.
“[This research provides] an option for pregnant women who don’t want to start antiretrovirals early.”
James Tumwine, Makerere University
To prevent mother-to-child HIV transmission, the WHO currently recommends a treatment approach known as Option B+. This involves treating HIV positive pregnant women with antiretroviral drugs regardless of their virus count, and giving their babies the drugs for up to six weeks to prevent infection.
But many HIV positive women are reluctant to take antiretrovirals because of their side effects and because they still feel healthy, according to James Tumwine, a child health researcher at Makerere University who led the part of the study done in Uganda. Antiretroviral drugs are given in lower doses when used to prevent rather than treat HIV, so children receive light doses with fewer side effects.
“[This research provides] an option for pregnant women who don’t want to start antiretrovirals early,” Tumwine says. “They can use these medicines for their children.”
The study, published in The Lancet on 18 November, analysed 1,236 babies of HIV positive mothers in Burkina Faso, South Africa, Uganda and Zambia between November 2009 and May 2012. The researchers gave HIV negative children antiretrovirals for up to 50 weeks to see if this would reduce virus transmission by more than giving them drugs for six weeks, as with Option B+.
Mothers reported their own breastfeeding habits, but the children were checked every three months to ensure they were being given the drugs. Over the study period, only 17 infants got infected with HIV, mostly because the drug regime was not followed, the researchers say.
Judith Kose, the senior technical officer for child HIV at the Elizabeth Glaser Pediatric AIDS Foundation in the United States, says that the long study period makes the research important, given that most mothers in the region breastfeed for around a year. “There is an element of benefit of being supported longer and being taught more about adherence and understanding the disease better,” she says.
But Kose points out that 50 weeks of therapy for the baby requires mothers to attend maternal clinics for longer, which reduces their economic activity and raises local health costs.The study’s findings are relevant to improving the current WHO method of preventing mother-to-child HIV transmissions, which focuses primarily on treating mothers, the paper says. But Sabrina Kitaka, a paediatrician at Makerere University, says the results cannot be directly compared with Option B+, because of the timing of its introduction.
“WHO guidelines for Option B+ came into force after this study,” she explains. “They were launched in July 2013, and in Uganda we took them up in October 2013”, meaning the study did not include babies enrolled in Option B+ for comparison.
The researchers intend to follow up the children to assess any long-term health impact of being given antiretroviral drugs for 50 weeks.
References
Nicolas Nagot and others Extended pre-exposure prophylaxis with lopinavir-ritonavir versus lamivudine to prevent HIV-1 transmission through breastfeeding up to 50 weeks in infants in Africa (ANRS 12174): a randomised controlled trial (The Lancet, 18 November 2015)