By: Joshua Howgego
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
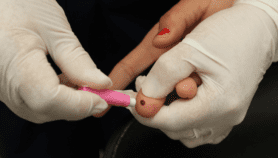
Giving sex workers HIV drugs before they are at risk of infection — in a strategy called pre-exposure prophylaxis (PrEP) — is showing promise as a public health strategy, a Guardian report highlighted recently. [1]
Female sex workers in insalubrious parts of the Kenyan city of Kisumu can often double their wages (to the equivalent of 24 US cents) if they agree to sex without a condom, putting themselves at risk of contracting HIV. Yet when they go to clinics the next day looking for drugs to fight a potential infection, they may be turned away due to social stigma, the Guardian reported. PrEP can potentially avoid this problem and, regardless, it’s more effective than post-exposure treatment.
But what’s less clear is how best to make these drugs available. Behavioural scientist Ana Wheelock, who is based at Imperial College London, United Kingdom, has spent several years investigating this question. [2] She says clinical trials have already proven that the treatment is effective, but what is now needed is to explore whether people will find the treatment regimes workable in real-life settings.
“PrEP is for women, men and transgender people at risk of infection who have made the informed decision to opt for that prevention method from a pool of different alternatives.”
Ana Wheelock, Imperial College London
“Oral PrEP is a promising HIV prevention method, particularly for women,” she says. “But we still do not know if people will adhere long term to the treatment regime as they need to in order to have the required level of protection.”
To answer that question, Wheelock explains, researchers are running ‘demonstration projects’ to evaluate the viability of PrEP and its possible economic advantages for a nation under realistic conditions. “Everyday life is different from a clinical trial, which is a very controlled environment,” she says.
For example, says Wheelock, if people know they are taking part in an experiment, they may be more likely to adhere to a treatment regime in order to fulfil their obligation. She adds that people who enrol in clinical trials are generally self-selected and so may be more motivated than the general population, and that clinical trials often provide targeted counselling and support, which may not be as comprehensive in public health programmes.
But these demonstration projects are not just about women who cannot negotiate the use of condoms, she tells me — and thinking about PrEP in that light would be a mistake.
“PrEP is for women, men and transgender people at risk of infection who have made the informed decision to opt for that prevention method from a pool of different alternatives,” she says. “PrEP, however, is not as innocuous and cheap as condoms. Thus, countries may need to prioritise certain groups, depending on their HIV epidemic.”
There are currently at least ten PrEP demonstration projects going on around the world — six in developing countries — including one looking at transgender people in India. [3]
They offer participants a “menu of choices that meet the needs of different groups”, says Wheelock, with PrEP being offered in conjunction with other options such as circumcision or antiretroviral drugs for HIV positive partners.
Joshua Howgego is deputy news and online editor at SciDev.Net. @jdhowgego
References
[1] Maurine Murenga and Corin Faife Kenyan sex workers using HIV drugs instead of condoms (The Guardian, 7 May 2014)
[2] Andreas B. Eisingerich, Ana Wheelock and others Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study (PLOS One, 11 January 2012)
[3] Ongoing and planned PrEP trials and demonstration projects, as of December 2013 (AVAC, December 2013)