By: Deodatus Balile
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
[DAR ES SALAAM] Larvicides could be back on the malaria control agenda after researchers in Tanzania found that killing mosquitoes before adulthood could cut malaria infection rates in urban areas.
The use of larvicides died out in developing countries with the introduction of the pesticide DDT (Dichloro-Diphenyl-Trichloroethane) in the mid-twentieth century. Their use has since been controversial due to concerns that larviciding is expensive and unsustainable.
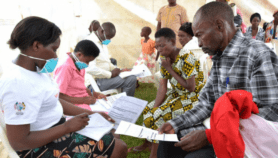
A team led by Gerry Killeen, from Tanzania’s Ifakara Health Institute, worked with the Dar es Salaam City Council for three years to develop the best ways of applying Bacillus thuringiensis israelensis (Bti) and Bacillus sphaericus (Bs) larvicides. Both are soil bacteria that kill mosquito larvae without being toxic to humans.
Three wards — Buguruni, Kurasini and Mikocheni — with 128,000 inhabitants were chosen to trial the larvicides for one year. Bti was added to outdoor ponds and swamps, and Bs was used to treat pit latrines, septic tanks and domestic sewerage systems.
The larvicides cut both the number of mosquitoes and the prevalence of malaria. Malaria rates in children under five decreased by 72 per cent and the researchers say the effect was as good as sleeping under an insecticide-treated bednet (ITN).
The method has been extended to cover 600,000 residents in thirty wards.
"I can’t tell the amount of mosquitoes we used to have here," says Salim Said, a resident of Buguruni. "They have helped us to do away with this nuisance."
Malaria control programmes usually focus on rural, high-risk areas but half of Africa’s population is expected to live in towns or cities by 2030 and controlling or eradicating malaria in such areas could be fairly easy, said Killeen.
Khadija Kannady, project manager of the Urban Malaria Control Programme (UMCP) which carried out the work, says using larvicides is viable and cost-effective since it costs US$0.5 cents to protect a person per year compared with US$2 for ITNs — but the two approaches should be complementary.
Prosper Chaki from Ifakara Health Institute, who was also involved in the research, says that the cooperation of the local community is important, and larvicide application is sometimes missed because of lack of access to property.
The research was published in PLoS ONE last month (31 March).
References
PLoS ONE doi 10.1371/journal.pone.0005107 (2009)