By: Carol Campbell
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Research into HIV treatment programmes in Africa found that over one third of people on antiretroviral therapy (ART) discontinue treatment within two years.
The findings were published in the October issue of PLoS Medicine.
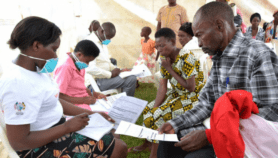
Researchers from the University of the Witwatersrand Health Consortium in Johannesburg, South Africa, and the United States investigated how long adult patients stayed in ART programmes in 13 Sub-Saharan African countries. They reviewed 32 reports published between 2000 and 2007.
Patient retention after two years varied widely, from 46 per cent to 85 per cent in the worst and best programmes. The average retention rate after two years was 61.6 per cent.
Almost half the lost patients died, often because treatment began too late. The rest were ‘lost to follow up’, either through unreported deaths or because they dropped out of treatment because of, for example, the high cost of treatment, long distances to the clinic and fear of stigma.
Programmes with high retention rates could be models for others, say the authors.
"Better patient tracing procedures, better understanding of loss to follow-up and earlier initiation of ART to reduce mortality are needed if retention is to be improved," they write.
Mary-Louise Newell, director of the Africa Centre for Health and Population Studies in South Africa’s KwaZulu Natal province, said her centre worked continuously to inform people that ART was a lifelong commitment.
"There has to be follow-up from caregivers for an ART programme to work effectively," she said.
The Africa Centre asks for patients’ contact details and uses road shows involving music and dance to spread information about ART among the rural, largely Zulu community it serves. "We see very low levels of loss to follow-up," said Newell.
Graham Cooke, a research physician with the centre, told SciDev.Net that they have reduced patients’ average travel distance from 37 kilometres to under 3 kilometres by establishing small, local clinics. As patients’ health improved, he said, others often came forward to ask for drugs. But he acknowledged that "mortality remains unacceptably high".
Cooke added that the centre’s approach to retaining patients worked on a local scale, but may not be applicable elsewhere in Africa.
Link to full paper in PLoS Medicine
Reference: PLoS Medicine doi 10.1371/journal.pmed.0040298 (2007)