By: Aamna Mohdin
Send to a friend
The details you provide on this page will not be used to send unsolicited email, and will not be sold to a 3rd party. See privacy policy.
Genetic information that could help slow disease outbreaks may be kept private by researchers out of fear of violating patients’ rights — that was one of the concerns expressed in a Nature article recently. [1]
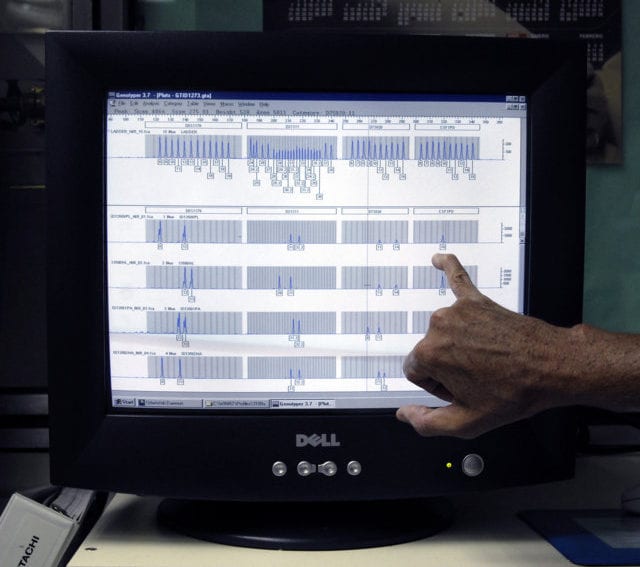
At the height of the Ebola epidemic, the authors of the piece sequenced 99 Ebola genomes from patients in Sierra Leone. The data was immediately uploaded to the public database GenBank and led to a surge in collaborations that eventually confirmed the virus had spread from Guinea to Sierra Leone, and indicated that the outbreak was being sustained by human-to-human transmission.
But the researchers wrote of a slump in the numbers of Ebola virus genomes isolated from patients and uploaded to open data repositories after theirs in mid-2014. That’s problematic, since the open sharing of data is essential to designing effective responses to outbreaks.
“In Africa, decision-making is a more communal process.”
Jantina De Vries, Human Heredity and Health in Africa
The researchers argued that one of the biggest barriers to open sharing of genetic data during health crises is the lack of coherent, internationally recognised guidelines on gaining informed consent from patients. Although such data is routinely anonymised, it’s still theoretically possible to identify participants from it. So scientists might avoid sharing genetic data they collect for fear that it could be misconstrued and used to stigmatise vulnerable populations. This might have partly caused the mid-2014 slump.
The authors suggest convening an international meeting involving health agencies, governments, biosecurity experts and ethicists to discuss what guidelines for informed consent could look like in emergency situations in developing nations.
I spoke to Jantina De Vries, the chair of the ethics committee working group at Human Heredity and Health in Africa (H3Africa), an organisation that has already developed guidelines on gaining informed consent on the continent. [2] She identifies three important issues that would have to be factored into any such guidelines.
First, De Vries says researchers have to move away from a “Western” understanding of autonomy in decision making, and create consent processes that are appropriate for local cultures. “In Africa, decision-making is a more communal process,” she says, explaining that usually, to enrol someone into medical research you would start by consulting at the community level, then the head of a household and only then would you approach an individual.
Second, she says consent processes should be accompanied by appropriate forms of community engagement that explain the research. For example, H3Africa is developing tools such as comic books, films and brochures to explain genetics and heredity.
“In fact, NGOs and patient advocacy groups were involved in the design of several research projects focusing on Ebola in the past few months.”
Jantina De Vries, Human Heredity and Health in Africa
Yet De Vries admits that different models would need to be used in an emergency, where researchers are trying to gather outbreak data fast. She tells me this is when community health workers and patient advocacy groups could play an important role. With the right training, these groups can help design the consent process, consent forms, and also assist in data collection — even in emergency situations.
“In fact, NGOs and patient advocacy groups were involved in the design of several research projects focusing on Ebola in the past few months,” says De Vries.
Last, is the issue of consent. H3Africa’s guidelines emphasise that researchers should explicitly mention that participants’ data might be shared in other research. Researchers can do this through a layered consent approach, where they first seek consent for the primary study, and then later for sharing sample with other researchers. De Vries suggests this approach is fairer where the research project offers access to better medical care than is on offer in the healthcare system, because participants are able to be involved in the medical research but can still choose not to have their sample shared further.
In terms of putting this into practice, De Vries suggests that “ethics consultations” with people from various ethics committees could be useful for quickly getting a local consensus on informed consent and data sharing. It is a model that H3Africa already follows, she says. “These consultations give us great feedback on whether certain policies would work, identify where the bottlenecks are, and decide what needs to be done both locally and internationally.”
Aamna Mohdin is a freelance journalist based in London. @aamnamohdin
References
[1] Nathan L. Yozwiak and others Data sharing: make outbreak research open access (Nature, 2015)
[2] H3Africa Guidelines for informed consent. Available from H3Africa Informed consent (H3Africa, 2013)